
Laboratory Animal and Comparative Medicine
• XXXX XXXX •
LIN Zhenhua( ), CHU Xiangyu(
), CHU Xiangyu( )(
)( ), WEI Zhenxi, DONG Chuanjun, ZHAO Zenglin, SUN Xiaoxia, LI Qingyu, ZHANG Qi
), WEI Zhenxi, DONG Chuanjun, ZHAO Zenglin, SUN Xiaoxia, LI Qingyu, ZHANG Qi
Online:2025-05-14
Contact:
CHU Xiangyu
CLC Number:
LIN Zhenhua,CHU Xiangyu,WEI Zhenxi,et al. Evaluation of the safety and efficacy of bone cement in experimental pigs using vertebroplasty[J]. Laboratory Animal and Comparative Medicine. DOI: 10.12300/j.issn.1674-5817.2025.006.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.slarc.org.cn/dwyx/EN/10.12300/j.issn.1674-5817.2025.006
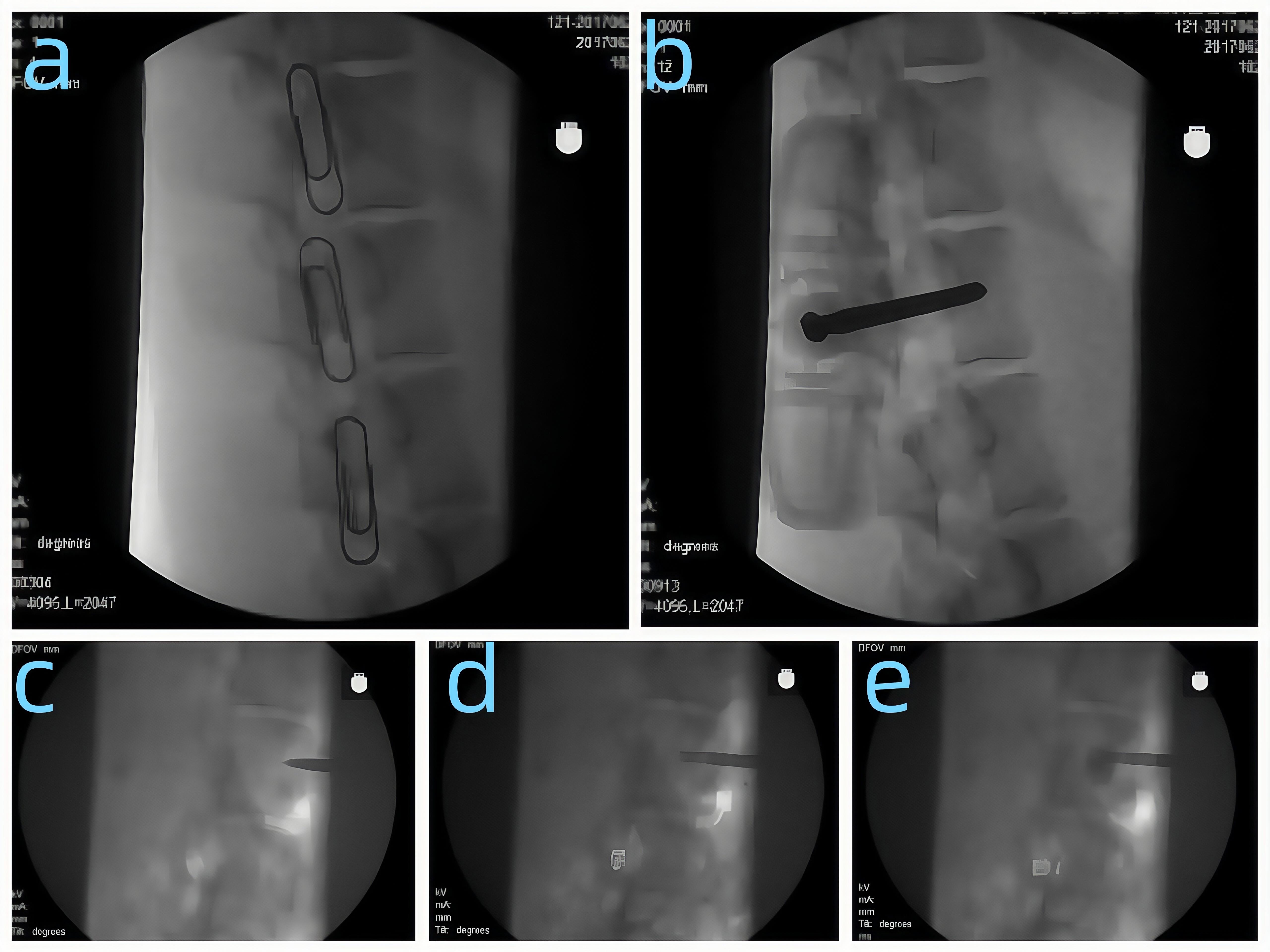
Figure 1 X-ray imaging picturesNote:a Locate the puncture site; b, The puncture needle reaches the target point (lateral view); c, The puncture needle reaches the target point (anteroposterior view); d, The bone cement injector enters the vertebral body; e, Bone cement is injected into the porcine vertebral body.
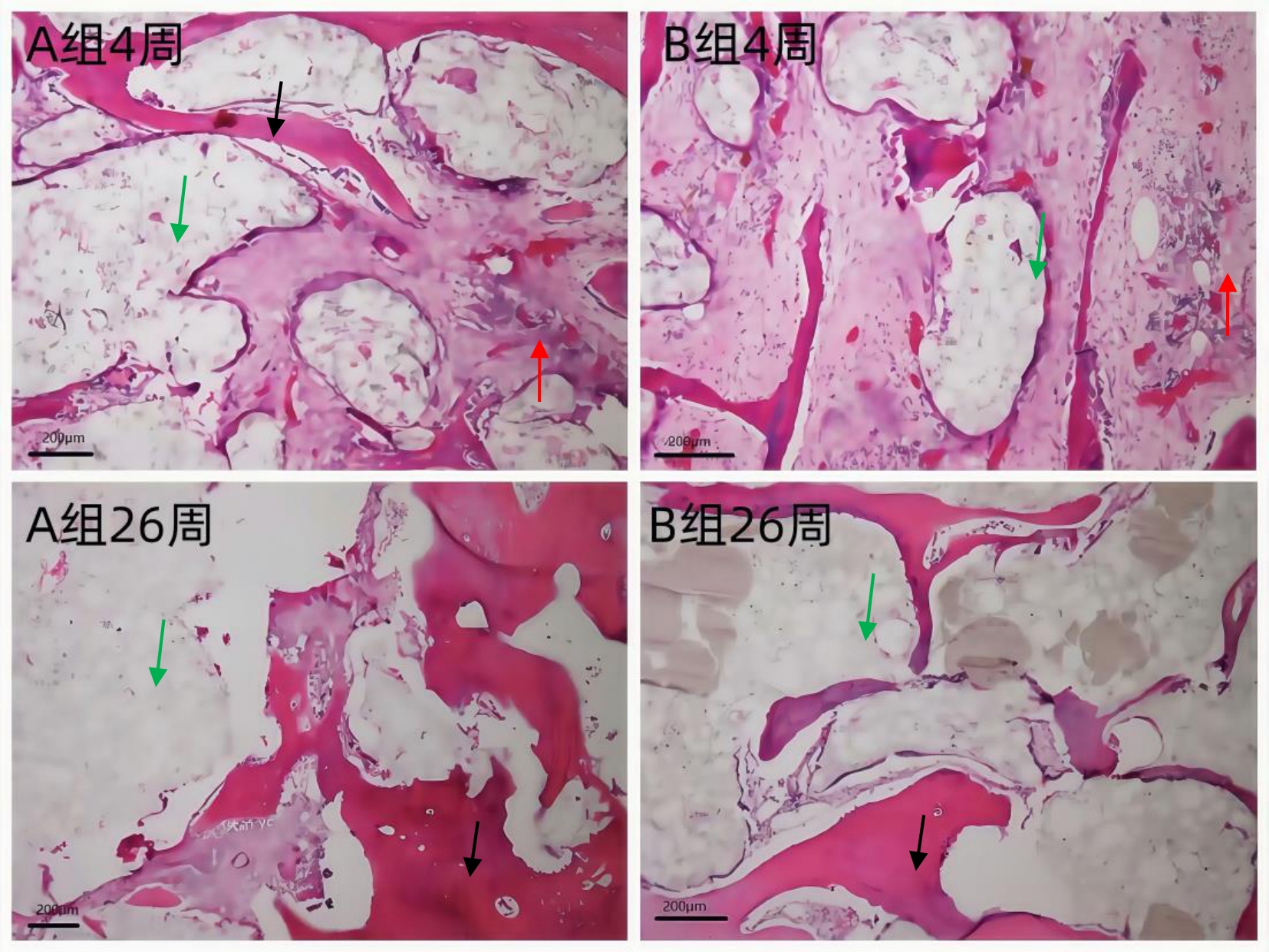
Figure 2 HE - stained pathological picture (×100)Note:In the area indicated by the red arrow, inflammatory cell infiltration can be seen. The green arrow indicates the bone cement, and the black arrow indicates the bone trabecula.
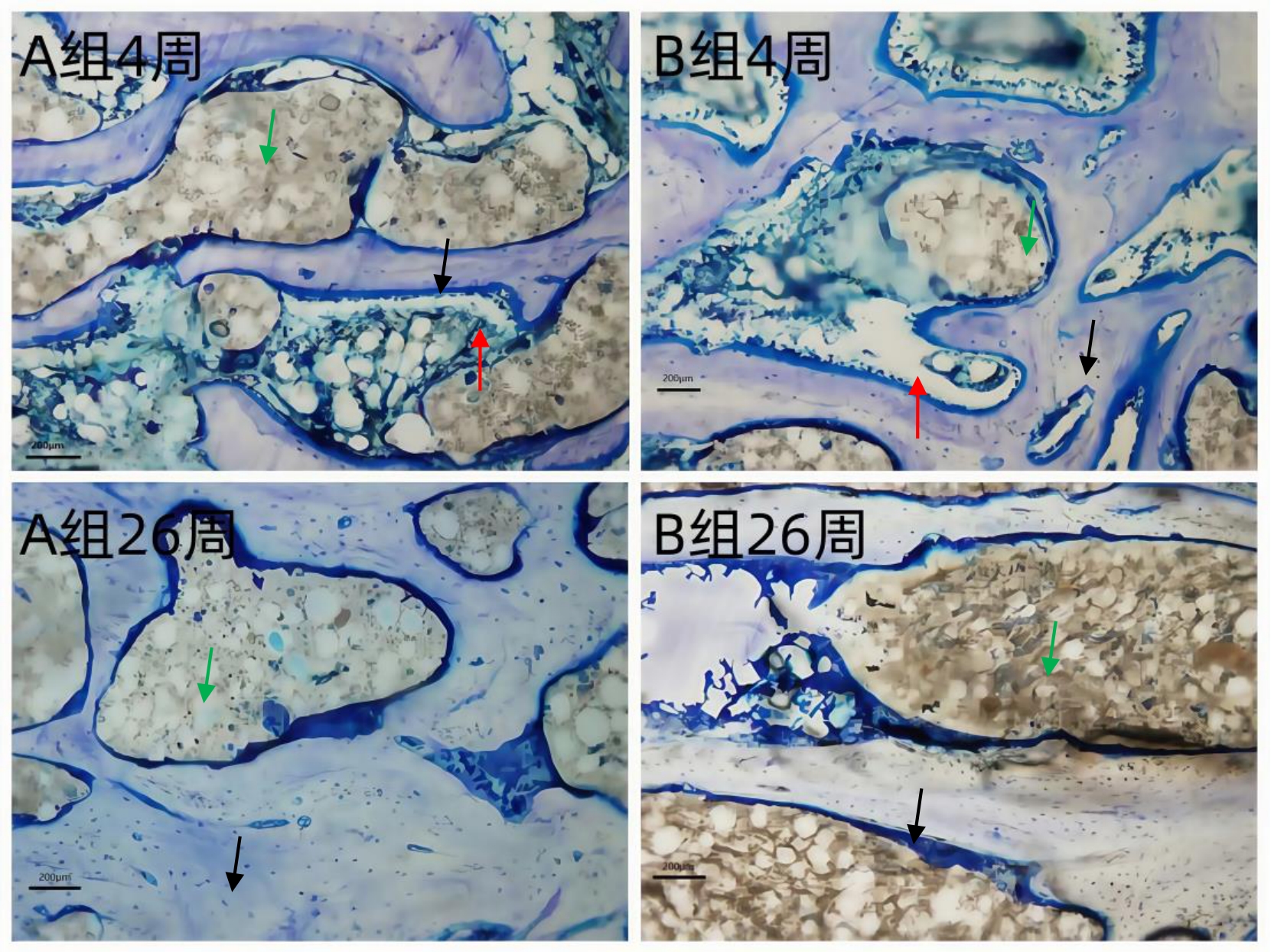
Figure 3 Toluidine blue - stained pathological picture (×100)3讨论Note:The area indicated by the red arrow is the osteoblast. The green arrow indicates the bone cement, and the black arrow indicates the bone trabecula.
| 1 | ZHANG Y, WANG X, LI Y, et al. Efficacy and safety of percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis [J]. BMC Musculoskelet Disord, 2023, 24 (1): 102. |
| 2 | LIU X, CHEN Y, ZHANG J, et al. Comparison of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a propensity score-matched analysis [J]. Eur Spine J, 2022, 31 (11): 2777-2784. |
| 3 | WANG Y, ZHAO Y, LIU X, et al. Risk factors for adjacent vertebral fractures after percutaneous vertebroplasty in osteoporotic vertebral compression fractures: a meta-analysis [J]. Spine J, 2021, 21 (12): 2641-2650. |
| 4 | 李波, 宁宁, 刘晓雪, 等. 不同骨水泥在椎体成形术中的应用进展[J]. 中国修复重建外科杂志, 2019, 33(1): 112-118. |
| LI B, NING N, LIU X X, et al. Application progress of different bone cements in vertebroplasty [J]. Chinese Journal of Reparative and Reconstructive Surgery, 2019, 33(1): 112-118. | |
| 5 | 李华,王伟,赵亮,等。经皮穿刺椎体成形术治疗骨质疏松性椎体压缩骨折的临床疗效及影响因素分析 [J]. 中华骨质疏松和骨矿盐疾病杂志,2023, 16 (2): 156-162. |
| LI H, WANG W, ZHAO L, et al. Analysis of the clinical efficacy and influencing factors of percutaneous vertebroplasty in the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Osteoporosis and Bone Mineral Research, 2023, 16(2): 156 - 162. | |
| 6 | 陈亮, 顾海伦, 原泉, 等. 聚甲基丙烯酸甲酯骨水泥对人骨髓间充质干细胞增殖及成骨分化的影响[J]. 中国脊柱脊髓杂志, 2013, 23(5): 446-452. |
| CHEN L, GU H L, YUAN Q, et al. Effects of polymethylmethacrylate bone cement on the proliferation and osteogenic differentiation of human bone marrow mesenchymal stem cells [J]. Chinese Journal of Spinal Cord and Spine, 2013, 23(5): 446 - 452. | |
| 7 | 赵燕鹏, 唐佩福, 张里程, 等. 磷酸钙骨水泥在椎体成形术中的应用[J]. 中国骨与关节杂志, 2015, 4(1): 62-66. |
| ZHAO Y P, TANG P F, ZHANG L C, et al. Application of calcium phosphate bone cement in vertebroplasty [J]. Chinese Journal of Bone and Joint, 2015, 4(1): 62 - 66. | |
| 8 | 王丽,张辉,刘畅,等。不同骨水泥在经皮穿刺椎体成形术中的应用效果比较 [J]. 中国矫形外科杂志,2022, 30 (18): 1673-1677. |
| WANG L, ZHANG H, LIU C, et al. Comparison of the application effects of different bone cements in percutaneous vertebroplasty [J]. Orthopedic Journal of China, 2022, 30(18): 1673 - 1677. | |
| 9 | 孙晓江, 杨述华, 孔清泉, 等. 新型可注射性骨水泥的生物力学及生物相容性研究[J]. 中国矫形外科杂志, 2008, 16(3): 208-211. |
| SUN X J, YANG S H, KONG Q Q, et al. Study on the biomechanics and biocompatibility of a novel injectable bone cement [J]. Orthopedic Journal of China, 2008, 16(3): 208 - 211. | |
| 10 | 朱悦, 阮狄克. 脊柱外科新手术剖析[M]. 辽宁科学技术出版社, 2005. |
| ZHU Y, RUAN D K. Analysis of New Operations in Spinal Surgery[M]. Liaoning Science and Technology Press, 2005. | |
| 11 | 汤亭亭, 戴尅戎. 骨水泥的生物力学及生物学性能[J]. 中国医疗器械杂志, 2001, 25(5): 283-286. |
| TANG T T, DAI K R. Biomechanical and Biological Properties of Bone Cement [J]. Chinese Journal of Medical Instrumentation, 2001, 25(5): 283 - 286. | |
| 12 | 刘训伟 等. 骨填充网袋修复椎体压缩性骨折的生物力学变化[J]. 中国组织工程研究,2014,04(16):2487-2492. |
| LIU X W, et al. Biomechanical changes of vertebral compression fractures repaired by bone filling mesh bags [J]. Chinese Journal of Tissue Engineering Research, 2014, 4(16): 2487 - 2492. | |
| 13 | 王亮, 许建中, 周强, 等. 经皮椎体成形术和椎体后凸成形术治疗骨质疏松性椎体压缩骨折的对比研究[J]. 中国脊柱脊髓杂志, 2011, 21(1): 13-17. |
| WANG L, XU J Z, ZHOU Q, et al. Comparative study on percutaneous vertebroplasty and percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fractures [J]. Chinese Journal of Spinal Cord and Spine, 2011, 21(1): 13 - 17. | |
| 14 | SMITH J, JOHNSON A, BROWN T. The impact of 3D - printed personalized bone cement on the outcomes of total hip arthroplasty: a prospective randomized controlled trial[J]. Journal of Arthroplasty, 2022, 37(10): 3107 - 3114. |
| 15 | WANG Q, LI H, ZHANG L, et al. A review of the research progress of bone cement in intelligent drug - controlled release[J]. Journal of Biomedical Materials Research Part B: Applied Biomaterials, 2021, 109(8): 1780 - 1790. |
| 16 | LI S, ZHAO X, LIU Y, et al. Personalized bone cement fabricated by 3D printing for complex bone defect repair: a preclinical study[J]. Additive Manufacturing, 2022, 56: 102677. |
| 17 | 贺宝荣, 郝定均, 许正伟, 等. 骨质疏松性椎体压缩骨折行椎体成形术后再骨折的相关因素分析[J]. 中国脊柱脊髓杂志, 2012, 22(3): 210-214. |
| HE B R, HAO D J, XU Z W, et al. Analysis of related factors of refracture after vertebroplasty for osteoporotic vertebral compression fractures [J]. Chinese Journal of Spinal Cord and Spine, 2012, 22(3): 210 - 214. |
| [1] | TANG Yingen, FENG Yaxian, ZHONG Min, WEI Zhen, WANG Lie, LIU Diwen. Polymorphism and Tissue Expression Analysis of TYR and MC1R Genes in Guinea Pigs with Different Coat-Color Phenotypes [J]. Laboratory Animal and Comparative Medicine, 2025, 45(1): 21-29. |
| [2] | LIU Yishu, CAI Liping. Advances and Challenges of Using Experimental Pigs in Da Vinci Surgical Robot Training [J]. Laboratory Animal and Comparative Medicine, 2024, 44(6): 667-674. |
| [3] | TU Yingxin, JI Yilan, WANG Fei, YANG Dongming, WANG Dongdong, SUN Zhixin, DAI Yuexin, WANG Yanji, Guanghan KAN, WU Bin, ZHAO Deming, YANG Lifeng. Evaluation of Simulated Weightlessness Model of Hindlimb Unloading Miniature Pigs and Their Tissue Damage [J]. Laboratory Animal and Comparative Medicine, 2024, 44(5): 475-486. |
| [4] | ZHU Chan, ZHANG Dongliang, ZHAO Deli, SHI Xueqin, QIAN Lei, ZHANG Xuan, JIN Yan, DUAN Wei, QI Ruocheng, LIU Chaohua, YANG Xuekang, HAN Juntao, PAN Dengke. Perioperative Animal Care for Xenotransplantation from Genetically Edited Pigs to Monkeys [J]. Laboratory Animal and Comparative Medicine, 2024, 44(5): 495-501. |
| [5] | LIU Kai, HU Yuqi, GENG Yatian, CHENG Wenjie, WANG Jing, WEI Taiyun, ZHAO Hongfang, LI Jiayu, JIAO Deling, ZHAO Hongye, WEI Hongjiang. Preliminary Study on Construction Method of Type 1 Diabetes Model in Banna Miniature Pig [J]. Laboratory Animal and Comparative Medicine, 2024, 44(4): 384-392. |
| [6] | Yishu LIU, Shanmin ZHAO, Liping CAI. Application and Comparison of Different Anesthetic Ventilation Methods in Minimally Invasive Thoracic Surgery Training [J]. Laboratory Animal and Comparative Medicine, 2024, 44(1): 97-104. |
| [7] | Jiaoxiang WANG, Yan WANG, Ke HU, Kaixiang XU, Taiyun WEI, Deling JIAO, Heng ZHAO, Hongye ZHAO, HongJiang WEI. Establishment of PCR Identification Method for Pig Blood Type [J]. Laboratory Animal and Comparative Medicine, 2023, 43(6): 585-594. |
| [8] | Shuzhen ZHANG, Yanguang ZHAO. Investigation Report on the Production and Utilization Status of Experimental Mini-pigs [J]. Laboratory Animal and Comparative Medicine, 2023, 43(5): 559-565. |
| [9] | Taofeng LU, Hui ZHANG, Jie ZHOU, Qian LI, Shuguang WU, Yanjun WU. Effects of Pogostemon cablin on Serum Metabolomiceof Guizhou Miniature Pigs and It's mechanism [J]. Laboratory Animal and Comparative Medicine, 2023, 43(3): 253-261. |
| [10] | Ying TAN, Wenping LIAO, Qilong GAO, Yong LI, Xinhui SHI, Jingkun WANG. Physiological Indexes and Histopathology Analysis of Sodium Iodate-Induced Retinitis Pigmentosa in Rats [J]. Laboratory Animal and Comparative Medicine, 2023, 43(2): 124-135. |
| [11] | Chen SHEN, Baojie ZHANG, Xuemin WANG, jinyan ZHU, Min ZHANG, Bin LI. Comparison of the Anesthetic Effects of Different Doses of Ketamine Hydrochloride Combined Xylazine on Short-term Anesthesia in Bama Miniature Pigs [J]. Laboratory Animal and Comparative Medicine, 2022, 42(3): 262-265. |
| [12] | Chang WU, Xiaojie LI, Yinnan WU, Yao WANG, Yuxin WANG, Weifeng ZONG, Changhong MENG, Yihong LU. Application of Isolated Guinea Pig Ileum Method for Detection of Histamine Substances in Osteopeptide Injections [J]. Laboratory Animal and Comparative Medicine, 2022, 42(2): 159-165. |
| [13] | Laien XUE. Anesthetic Effects of Zoletil and Xylazine on Bama Mini-pigs [J]. Laboratory Animal and Comparative Medicine, 2022, 42(1): 26-30. |
| [14] | XIAO Pan, NIU Tingxian, LUO Xiaohong, WANG Hongyi, GUO Xiaoyu, LU Lu, FENG Xiaoming. Changes of C-reactive Protein and Inflammatory Factors in Juema Pig Model with High Altitude Multiple Organ Dysfunction Syndrome [J]. Laboratory Animal and Comparative Medicine, 2021, 41(3): 238-243. |
| [15] | ZHANG Hui, WU Yanjun, YAO Jin, LU Taofeng, WANG Guoqi, ZHAO Hai, YAO Gang, WU Shuguang. Therapeutic Effect of Wuling Powder on Guizhou Mini-pigs of Hyperlipidemia Model [J]. Laboratory Animal and Comparative Medicine, 2021, 41(2): 138-142. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||