
Laboratory Animal and Comparative Medicine ›› 2024, Vol. 44 ›› Issue (5): 543-549.DOI: 10.12300/j.issn.1674-5817.2024.044
• Animal Models of Human Diseases • Previous Articles Next Articles
ZHANG Naiqun1( ), YUAN Piaopiao1, CAO Linrong1, YING Na1, YANG Taotao2(
), YUAN Piaopiao1, CAO Linrong1, YING Na1, YANG Taotao2( )(
)( )
)
Received:2024-03-13
Revised:2024-08-04
Online:2024-10-25
Published:2024-11-06
Contact:
YANG Taotao
CLC Number:
ZHANG Naiqun,YUAN Piaopiao,CAO Linrong,et al. Application of PNR Detection in the Diagnosis and Drug-efficacy Evaluation of Diabetic Kidney Disease in Rats[J]. Laboratory Animal and Comparative Medicine, 2024, 44(5): 543-549. DOI: 10.12300/j.issn.1674-5817.2024.044.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.slarc.org.cn/dwyx/EN/10.12300/j.issn.1674-5817.2024.044
造模后时间 Time after molding/d | U-ACR/(mg·g-1) | PNR | |||
|---|---|---|---|---|---|
正常组 Normal | 模型组 Model | 正常组 Normal | 模型组 Model | ||
| 3 | 12.69±3.69 | ND | 0.85±0.40 | 0.39±0.19 | |
| 5 | 13.29±4.05 | ND | 0.88±0.31 | 0.64±0.45 | |
| 7 | 13.02±3.7 | ND | 0.86±0.37 | 0.66±0.10 | |
| 9 | 12.14±3.27 | 9.45±6.23 | 0.91±0.27 | 1.26±0.11 | |
| 11 | 11.96±3.21 | 18.19±8.75 | 0.90±0.25 | 1.70±0.65 | |
| 13 | 13.88±4.02 | ND | 0.89±0.30 | 1.63±0.63 | |
| 15 | 12.73±3.98 | 72.59±19.51 | 0.87±0.38 | 1.25±0.17 | |
| 17 | 13.01±2.98 | 77.68±11.16 | 0.91±0.42 | 2.54±0.20 | |
Table 1 Changes of U-ACR and PNR values in rats after STZ modeling
造模后时间 Time after molding/d | U-ACR/(mg·g-1) | PNR | |||
|---|---|---|---|---|---|
正常组 Normal | 模型组 Model | 正常组 Normal | 模型组 Model | ||
| 3 | 12.69±3.69 | ND | 0.85±0.40 | 0.39±0.19 | |
| 5 | 13.29±4.05 | ND | 0.88±0.31 | 0.64±0.45 | |
| 7 | 13.02±3.7 | ND | 0.86±0.37 | 0.66±0.10 | |
| 9 | 12.14±3.27 | 9.45±6.23 | 0.91±0.27 | 1.26±0.11 | |
| 11 | 11.96±3.21 | 18.19±8.75 | 0.90±0.25 | 1.70±0.65 | |
| 13 | 13.88±4.02 | ND | 0.89±0.30 | 1.63±0.63 | |
| 15 | 12.73±3.98 | 72.59±19.51 | 0.87±0.38 | 1.25±0.17 | |
| 17 | 13.01±2.98 | 77.68±11.16 | 0.91±0.42 | 2.54±0.20 | |
组别 Group | U-ACR/(mg·g-1) | PNR | |||
|---|---|---|---|---|---|
给药前 0 week | 给药4周 4 weeks | 给药前 0 week | 给药4周 4 weeks | ||
正常对照 Normal control (0.9%NS) | 11.69±3.15 | 11.45±3.25 | 0.92±0.21 | 0.89±0.17 | |
模型对照 Model control (0.9%NS) | 17.96±6.45 | 896.12±62.89 ** | 1.24±0.11 | 1.64±0.08 ** | |
缬沙坦低剂量 Valsartan 25 mg/kg | 18.08±7.03 | 408.99±78.03 △△ | 1.16±0.14 | 0.53±0.13 △△ | |
缬沙坦高剂量 Valsartan 50 mg/kg | 18.86±6.90 | 480.97±94.34 △△ | 1.14±0.24 | 1.28±0.44 | |
福辛普利钠低剂量 Fosinopril 30 mg/kg | 18.73±6.82 | 314.93±67.81 △△ | 1.26±0.22 | 0.92±0.28 △△ | |
福辛普利钠高剂量 Fosinopril 60 mg/kg | 17.86±5.92 | 236.61±43.55 △△ | 1.17±0.21 | 2.14±0.29 | |
Table 2 Effects of drug intervention on U-ACR and PNR in diabetic model rats
组别 Group | U-ACR/(mg·g-1) | PNR | |||
|---|---|---|---|---|---|
给药前 0 week | 给药4周 4 weeks | 给药前 0 week | 给药4周 4 weeks | ||
正常对照 Normal control (0.9%NS) | 11.69±3.15 | 11.45±3.25 | 0.92±0.21 | 0.89±0.17 | |
模型对照 Model control (0.9%NS) | 17.96±6.45 | 896.12±62.89 ** | 1.24±0.11 | 1.64±0.08 ** | |
缬沙坦低剂量 Valsartan 25 mg/kg | 18.08±7.03 | 408.99±78.03 △△ | 1.16±0.14 | 0.53±0.13 △△ | |
缬沙坦高剂量 Valsartan 50 mg/kg | 18.86±6.90 | 480.97±94.34 △△ | 1.14±0.24 | 1.28±0.44 | |
福辛普利钠低剂量 Fosinopril 30 mg/kg | 18.73±6.82 | 314.93±67.81 △△ | 1.26±0.22 | 0.92±0.28 △△ | |
福辛普利钠高剂量 Fosinopril 60 mg/kg | 17.86±5.92 | 236.61±43.55 △△ | 1.17±0.21 | 2.14±0.29 | |
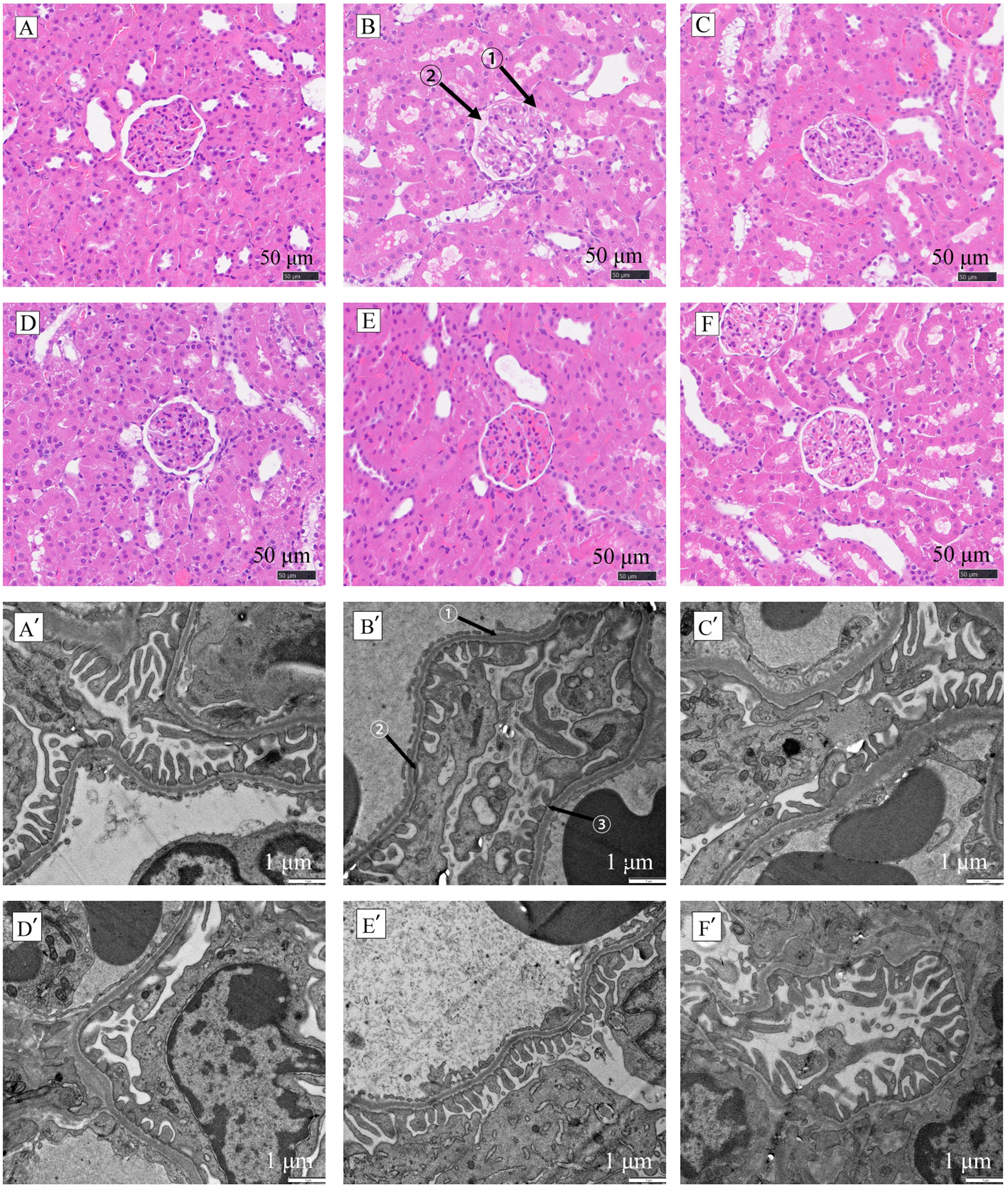
Figure 1 HE staining (A-F, ×400) and transmission electron microscopy (A'-F', ×5 000) of renal tissues in each group of ratsNote:A and A’ represent the normal control group (0.9% NaCl), B and B' represent the model control group (0.9% NaCl), C and C' represent the low-dose Valsartan group (Valsartan 25 mg/kg), and D and D' represent the high-dose Valsartan group (Valsartan 50 mg/kg). E and E' represent the low-dose fosinopril sodium group (Fosinopril 30 mg/kg), and F and F’represent the high-dose fosinopril sodium group (Fosinopril 60 mg/kg). In fig. B, the arrow ① indicates the glomerular contour, the arrow ② indicates the mesangial matrix deposition. In fig. B', the arrow ① indicates the diffuse irregular thickening of the podocyte membrane, while the arrows ② and ③ indicate damage and fuzziness of the “zipper” layout of podocytes.
| 1 | LUO J L, PIAO C L, JIN D, et al. Mechanism of rhubarb for diabetic kidney disease through the AMPK/NF-κB signaling pathway based on network pharmacology[J]. ChemistrySelect, 2022, 7(4): e202103534. DOI: 10.1002/slct.202103534 . |
| 2 | 杨涛涛, 陈民利. 足细胞蛋白Nephrin、Podocin与肾小球疾病[J]. 中国比较医学杂志, 2013, 23(11):72-77. DOI: 10.3969.j.issn.1671.7856.2013.011.016 . |
| YANG T T, CHEN M L. Podocyte protein nephrin, podocin and glomerulopathy[J]. Chin J Comp Med, 2013, 23(11):72-77. DOI: 10.3969.j.issn.1671.7856.2013.011.016 . | |
| 3 | 陈月梅, 张春莹, 龙婷婷, 等. 随机尿蛋白、尿蛋白/肌酐比值及尿微量白蛋白/肌酐比值在早期糖尿病肾病中应用价值[J]. 临床军医杂志, 2023, 51(4):362-365, 369. DOI:10.16680/j.1671-3826.2023.04.07 . |
| CHEN Y M, ZHANG C Y, LONG T T, et al. Application value of random urine protein,urinary albumin/urinary creatinine ratio and urine microalbumine creatinine ra-tio in early diabetic nephropathy[J]. Clin J Med Off, 2023,51(4):362-365, 369. DOI:10.16680/j.1671-3826.2023.04.07 . | |
| 4 | 叶桐江, 郑博文, 赵琳, 等. 链脲佐菌素诱导1型糖尿病大鼠模型的最佳禁食时间与最优剂量[J]. 兰州大学学报(医学版), 2019, 45(2):52-55. DOI: 10.13885/j.issn.1000-2812.2019.02.009 . |
| YE T J, ZHENG B W, ZHAO L, et al. Optimal fasting time and dose of streptozotocin-induced diabetic rat model[J]. J Lanzhou Univ Med Sci, 2019, 45(2):52-55. DOI: 10.13885/j.issn.1000-2812.2019.02.009 . | |
| 5 | 吴兆芳, 于艳丽, 韩红梅, 等. 2型糖尿病患者胰岛素抗体水平与尿白蛋白/肌酐比值的相关性研究[J]. 中国糖尿病杂志, 2022, 8(6):431-435. DOI: 10.3969/j.issn.1006-6187.2022.06.007 . |
| WU Z F, YU Y L, HAN H M, et al. Correlation between insulin antibody and urinary albumin/creatinine ratio in patients with type 2 diabetes mellitus[J]. Chin J Diabetes, 2022, 8(6):431-435. DOI: 10.3969/j.issn.1006-6187.2022.06.007 . | |
| 6 | 朱丽坤, 曹爽, 蒋仕林, 等. 黄芪注射液对db/db小鼠肾脏IL-1β、MCP-1和TNF-α的mRNA表达的影响[J]. 实验动物与比较医学, 2020, 40(1):60-64. DOI: 10.3969/j.issn.1674-5817.2020.01.010 . |
| ZHU L K, CAO S, JIANG S L, et al. Effect of Astragalus injection on mRNA expression of IL-1β, MCP-1 and TNF-α in kidney of db/db mice[J]. Lab Anim Comp Med, 2020, 40(1):60-64. DOI: 10.3969/j.issn.1674-5817.2020.01.010 . | |
| 7 | KOSTOVSKA I, TRAJKOVSKA K T, TOPUZOVSKA S, et al. Nephrinuria and podocytopathies[J]. Adv Clin Chem, 2022, 108:1-36. DOI: 10.1016/bs.acc.2021.08.001 . |
| 8 | 关冰, 田雪, 李伟男, 等. 健脾益肾活血方对膜性肾病大鼠肾组织Nephrin和Podocin表达的影响[J]. 现代中西医结合杂志, 2022, 8(6):731-736. |
| GUAN B, TIAN X, LI W N, et al. Effect of Jianpi Yishen Huoxue Decoction on the expression of Nephrin and Podocin in renal tissue of rats with membranous nephropathy[J]. Mod J Integr Tradit Chin West Med, 2022, 8(6):731-736. | |
| 9 | 吝娜, 曹磊, 王保兴. 舒洛地特对膜性肾病大鼠肾组织中podocin、nephrin表达的影响[J]. 临床内科杂志, 2022, 39(7):481-485. DOI: 10.3969/j.issn.1001-9057.2022.07.013 . |
| LIN N, CAO L, WANG B X. Effects of sulodexide on the expression of podocin and nephrin in renal tissues of membranous nephropathy rats[J]. J Clin Intern Med, 2022, 39(7):481-485. DOI: 10.3969/j.issn.1001-9057.2022.07.013 . | |
| 10 | SWAMINATHAN S M, RAO I R, SHENOY S V, et al. Novel biomarkers for prognosticating diabetic kidney disease progression[J]. Int Urol Nephrol, 2023, 55(4):913-928. DOI: 10.1007/s11255-022-03354-7 . |
| 11 | 罗文婷, 唐诗韵, 肖湘, 等. 糖尿病肾病动物模型的研究进展[J]. 成都医学院学报, 2023, 18(5):650-657. DOI: 10.3969/j.issn.1674-2257.2023.05.023 . |
| LUO W T, TANG S Y, XIAO X, et al. Research progress of animal models of diabetic nephropathy[J]. J Chengdu Med Coll, 2023, 18(5):650-657. DOI: 10.3969/j.issn.1674-2257.2023.05.023 . | |
| 12 | 王雪, 呼永河. 糖尿病小鼠模型的常见种类及其构建要素分析[J]. 实验动物与比较医学, 2023, 43(4):415-421. DOI: 10.12300/j.issn.1674-5817.2023.031 . |
| WANG X, HU Y H. Analysis of common types and construction elements of diabetic mouse models[J]. Lab Anim Comp Med, 2023, 43(4):415-421. DOI: 10.12300/j.issn.1674-5817.2023.031 . | |
| 13 | 程乾, 沈永芹, 谷雨, 等. 银杏叶提取物、卡托普利、缬沙坦单独用药及联合用药对高糖培养的大鼠肾小球系膜细胞的保护作用[J]. 徐州医学院学报, 2010(6):351-354. DOI: 10.3969/j.issn.1000-2065.2010.06.001 . |
| CHENG Q, SHEN Y Q, GU Y, et al. Cytoprotection of the monotherapy and combination treatment of Ginkgo biloba extract, captopril, valsartan on rat glomerular mesangial cells cultured in high glucose[J]. Acta Acad Med Xuzhou, 2010(6):351-354. DOI: 10.3969/j.issn.1000-2065.2010.06.001 . | |
| 14 | FUJIWARA T, YANO Y, HOSHIDE S, et al. 缬沙坦/氨氯地平联合治疗时夜间中心血压变化与尿白蛋白/肌酐的相关性[J]. 中华高血压杂志, 2019, 5(7):698. DOI: 10.16439/j.cnki.1673-7245.2019.07.028 . |
| FUJIWARA T, YANO Y, HOSHIDE S, et al. Association between change in central nocturnal blood pressure and urine albumin-creatinine ratio by a valsartan/amlodipine vombination: a CPET study[J]. Chin J Hypertens, 2019, 5(7):698. DOI: 10.16439/j.cnki.1673-7245.2019.07.028 . | |
| 15 | ANTAL-KONYA V, SCHAY G, KETSZERI M, et al. The regulation of the nephrin-nephrin distance by podocin mediates the interallelic interactions of the NPHS2 R229Q variant[J]. Pediatr Nephrol, 2023, 38(7):2262-2263. |
| 16 | 陈霞波, 龚文波, 陈民利, 等. 温肾健脾方对糖尿病肾病大鼠肾小球足细胞nephrin和podocin表达的影响[J]. 中华危重症医学杂志(电子版), 2017, 10(4):224-229. DOI: 10.3877/cma.j.issn.1674-6880.2017.04.003 . |
| CHEN X B, GONG W B, CHEN M L, et al. Effect of warming kidney and spleen recipe on the expressions of nephrin and podocin in glomerular podocyte of diabetic nephropathy rats[J]. Chin J Crit Care Med Electron Ed, 2017, 10(4):224-229. DOI: 10.3877/cma.j.issn.1674-6880.2017.04.003 . |
| [1] | YANG Jin, YU Shiya, LIN Nan, FANG Yongchao, ZHAO Hu, QIU Jinwei, LIN Hongming, CHEN Huiyan, WANG Yu, WU Weihang. Effect of Modified Duodenal Exclusion Surgery on Glucose Metabolism in Rats with Type 2 Diabetes Mellitus [J]. Laboratory Animal and Comparative Medicine, 2024, 44(5): 523-530. |
| [2] | QI Longju, CHEN Shiyuan, LIAO Zehua, SHI Yuanhu, SUN Yuyu, WANG Qinghua. Transcriptomic Analysis of Menstrual Blood-Derived Stem Cells Transplantation Combined with Exercise Training in Promoting Spinal Cord Injury Recovery in Rats [J]. Laboratory Animal and Comparative Medicine, 2024, 44(5): 531-542. |
| [3] | ZHENG Yiqing, DENG Yasheng, FAN Yanping, LIANG Tianwei, HUANG Hui, LIU Yonghui, NI Zhaobing, LIN Jiang. Application Analysis of Animal Models for Pelvic Inflammatory Disease Based on Data Mining [J]. Laboratory Animal and Comparative Medicine, 2024, 44(4): 405-418. |
| [4] | XIAO Pan, WANG Hongyi, LU Lu, ZHANG Mei, CHEN Keming, SHEN Dongshuai, NIU Tingxian. Screening of Hypoxia-Sensitive and Hypoxia-Tolerant Wistar Rats and Preliminary Exploration of Hypoxia Sensitivity in Their G1 Generation [J]. Laboratory Animal and Comparative Medicine, 2024, 44(4): 374-383. |
| [5] | Xiaoyu ZHU, Hantao YUAN, Sibo LI. MicroRNA-887-3p Inhibited MDM4 Expression and Proliferation but Promoted Apoptosis of Intervertebral Disc Annulus Fibrosus Cells in Rats [J]. Laboratory Animal and Comparative Medicine, 2024, 44(3): 270-278. |
| [6] | Jinhua HU, Jingjie HAN, Min JIN, Bin HU, Yuefen LOU. Effects of Puerarin on Bone Density in Rats and Mice: A Meta-analysis [J]. Laboratory Animal and Comparative Medicine, 2024, 44(2): 149-161. |
| [7] | Liya ZHAO, Liju NI, Caiqin ZHANG, Jianping TANG, Yangzheng YAO, Yanyan NIE, Xiaoxue GU, Ying ZHAO. Establishing a Genetic Detection Protocol of Single Nucleotide Polymorphisms Panels in Inbred Rats Based on Multiplex PCR-LDR [J]. Laboratory Animal and Comparative Medicine, 2023, 43(5): 548-558. |
| [8] | Lingzhi YU, Jianyun XIE, Liping FENG, Xiaofeng WEI. Establishment of Fluorescence qPCR Method for Detection of Staphylococcus Aureus and Its Application in Feces Detection of Rats and Mice [J]. Laboratory Animal and Comparative Medicine, 2023, 43(5): 566-573. |
| [9] | Ziyin XIA, Yuanyuan CHAI, Yunxia XU, Qinwei YU, Xin HUANG, Luyong ZHANG, Zhenzhou JIANG. Quantification of Uric Acid of Rat Serum by Liquid Chromatography-ultraviolet Detection and Its Comparison Study [J]. Laboratory Animal and Comparative Medicine, 2023, 43(3): 314-322. |
| [10] | Ying TAN, Wenping LIAO, Qilong GAO, Yong LI, Xinhui SHI, Jingkun WANG. Physiological Indexes and Histopathology Analysis of Sodium Iodate-Induced Retinitis Pigmentosa in Rats [J]. Laboratory Animal and Comparative Medicine, 2023, 43(2): 124-135. |
| [11] | Jian GE, Jingfen SUN, Yongjie WU. Taurine Has no Protective Effect on Rat Corneal Endothelial Cells Injured by Benzalkonium Chloride [J]. Laboratory Animal and Comparative Medicine, 2023, 43(1): 39-43. |
| [12] | Qin XU, Yan NI, Wenhui SHI, Jianying LI, Jiangwei LIU, Hongqiong ZHAO, Xinming XU. Analysis on Ileum and Colon Microflora of SPF Male SD Rats based on High-throughput Sequencing [J]. Laboratory Animal and Comparative Medicine, 2023, 43(1): 53-60. |
| [13] | Bin WU, Xu WANG, Dongxu FU, Yujun ZHU, Jinlu HUANG, Shunxing ZHU. Effect of the Traditional Chinese Medicine Shuganjieyu Formula on Constipation Type Irritable Bowel Syndrome and Brain-gut Axis in Rats [J]. Laboratory Animal and Comparative Medicine, 2022, 42(6): 551-559. |
| [14] | Chen GAO, Chunling FAN, Yurong LI, Wenjuan PEI, Caiping GUAN. Changes in Expression of Monocarboxylate Transporters in the Rat Cerebral Cortex after Exercise-induced Fatigue Under Simulated High-altitude Hypoxia and its Significance [J]. Laboratory Animal and Comparative Medicine, 2022, 42(5): 384-392. |
| [15] | Bingxin XU, Kaijian FAN, Tingyu WANG, Huijin CHEN. Effect of Dexamethasone on Cartilage Degeneration in Rats with Collagen-induced Arthritis [J]. Laboratory Animal and Comparative Medicine, 2022, 42(5): 416-422. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||