
Laboratory Animal and Comparative Medicine ›› 2022, Vol. 42 ›› Issue (4): 322-332.DOI: 10.12300/j.issn.1674-5817.2022.041
• Animal Models of Human Diseases • Previous Articles Next Articles
Yanbing ZHU1,2( ), Fan BAI3,4, Shaoxin TAO1,2, Yuhualei PAN1,2, Huan WANG1, Yushang ZHAO1, Song WANG1, Yan YU3,4(
), Fan BAI3,4, Shaoxin TAO1,2, Yuhualei PAN1,2, Huan WANG1, Yushang ZHAO1, Song WANG1, Yan YU3,4( )(
)( )
)
Received:2022-03-29
Revised:2022-05-19
Online:2022-08-25
Published:2022-08-25
Contact:
Yan YU
CLC Number:
Yanbing ZHU,Fan BAI,Shaoxin TAO,et al. Inhibition of Phospholipase D1 Activity Improves the Recovery of Neurological Function in Mice with Ischemic Stroke[J]. Laboratory Animal and Comparative Medicine, 2022, 42(4): 322-332. DOI: 10.12300/j.issn.1674-5817.2022.041.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.slarc.org.cn/dwyx/EN/10.12300/j.issn.1674-5817.2022.041
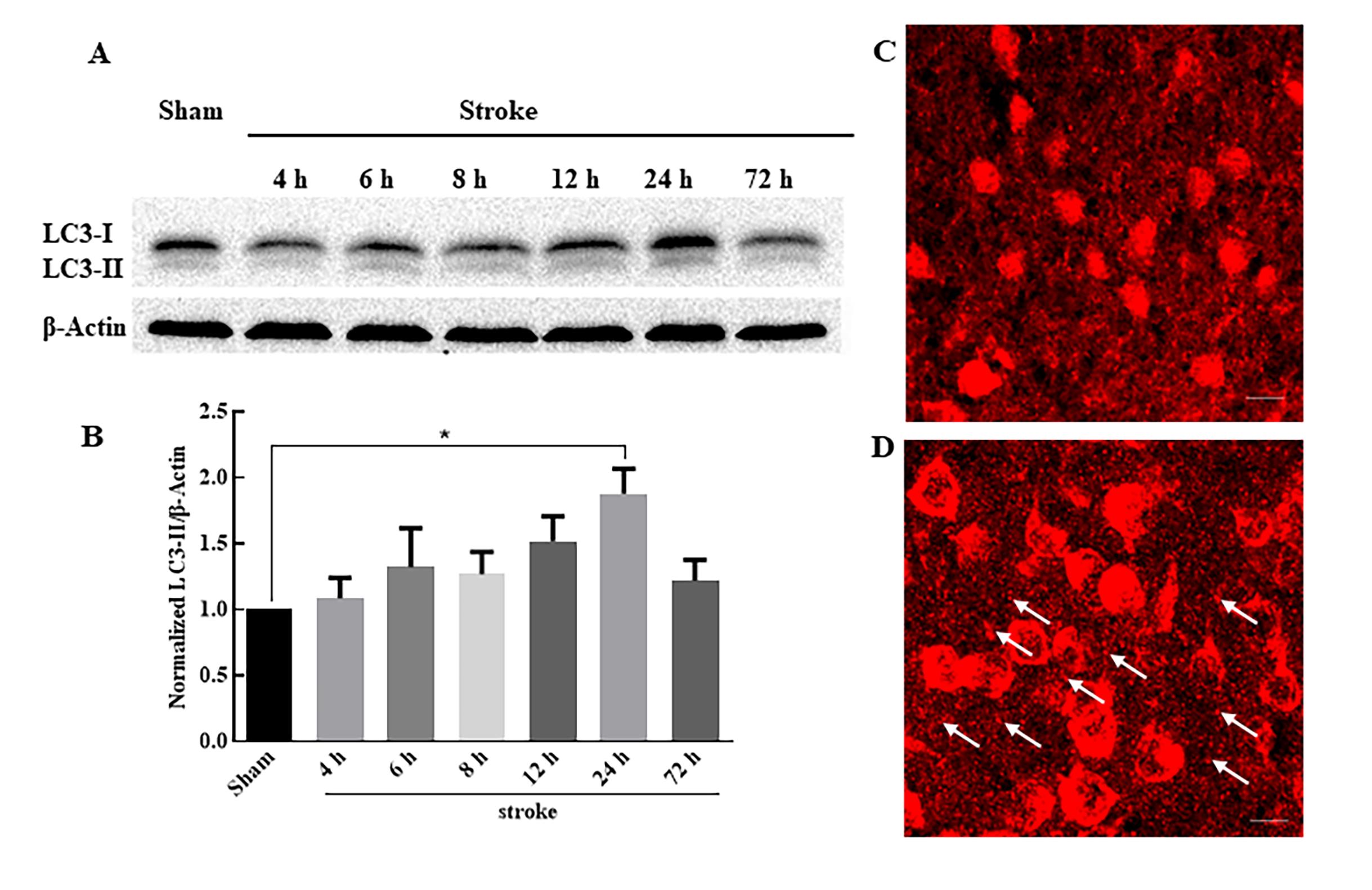
Figure 1 Expression of autophagy-related LC3 in the infracted cortex after ischemic stroke detected by Western blotting (A and B) and immunofluorescent staining (C and D)Note: A is the level of autophagy-related protein LC3 at different time points (4-72 h). B is the statistical analysis of the ratio of LC3-Ⅱ/β-actin at different time points (n=3 at each time point, *P<0.05). C is the morphology of LC3 in the sham group. D is the morphology of LC3 in 24-hour group after ischemic stroke (the arrow points for LC3-Ⅱ, and the scale bar is 10 μm).
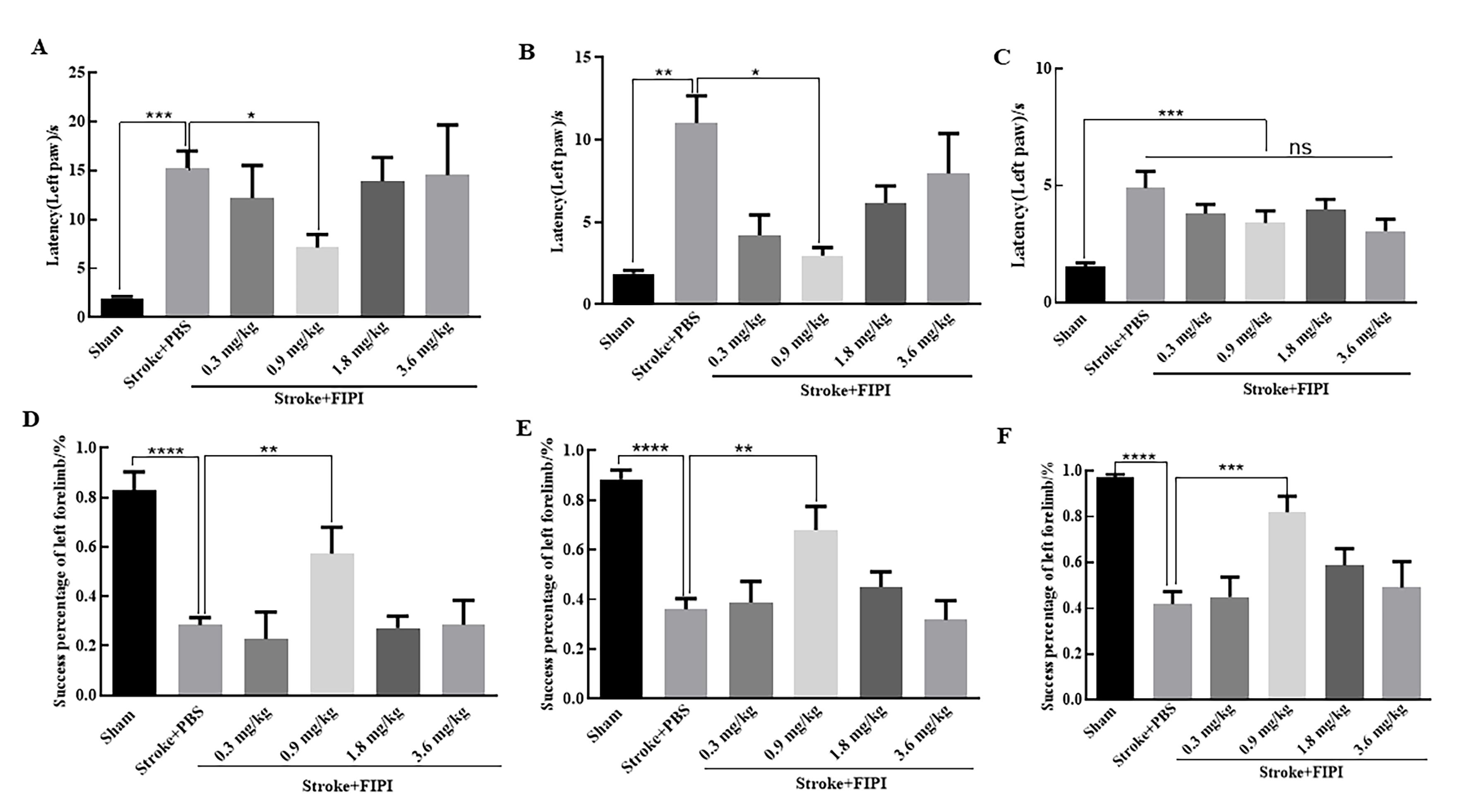
Figure 2 Behavior tests reveal administration of 0.9 mg/kg FIPI after ischemic stroke obviously improves neurological function of miceNote: A, B, and C denote adhesive removal tests (detecting latency time of left paw); D, E, and F are whisker tests (detecting success percentage of left forelimb). A and D show the behavior tests on the 1st day; B and E show the behavior tests on the 3rd day; C and F show the behavior tests on the 7th day. n=6 in each group; *P<0.05, **P<0.01, ***P<0.001, ****P<0.000 1; ns, not significant. FIPI, 5-fluoro-2-indolyl deschlorohalopemide, is a phospholipase D inhibitor.
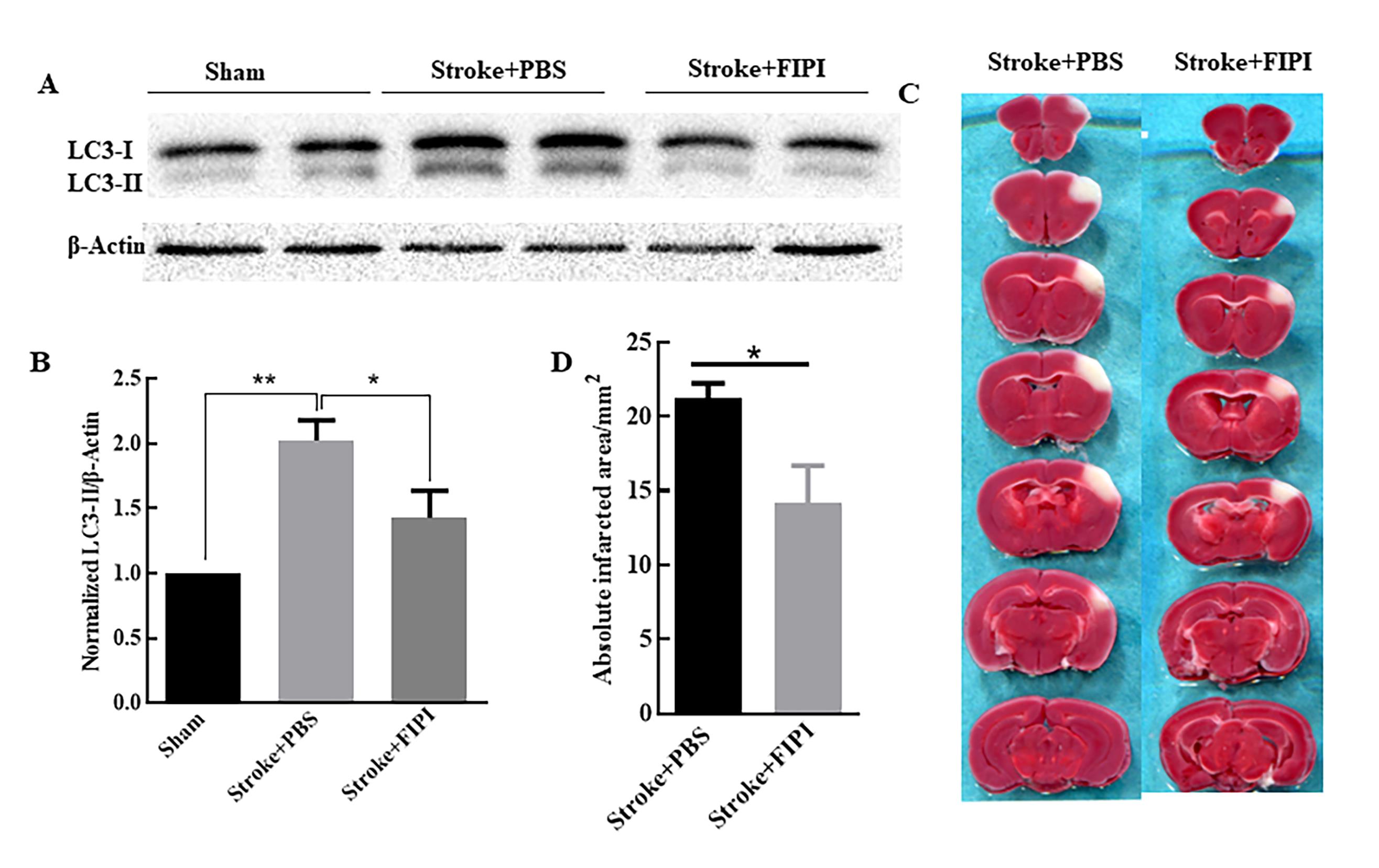
Figure 3 Expression of autophagy-related LC3 and the change in the infarcted cortex volume after FIPI inhibitor treatment are detected by Western blotting (A and B) and TTC staining (C and D)Note: A is the level of autophagy-related protein LC3 at different time points; B is the statistical analysis of the ratio of LC3-Ⅱ/β-actin (n=3 in each group, *P<0.05, **P<0.01). C is the TTC staining of the infarcted cortex in two groups; white color indicates the infarcted cortex and red color indicates the normal cortex; D is the statistical analysis of the infarcted cortex area (n=6 in each group, *P<0.05). FIPI, 5-fluoro-2-indolyl deschlorohalopemide, is a phospholipase D inhibitor.
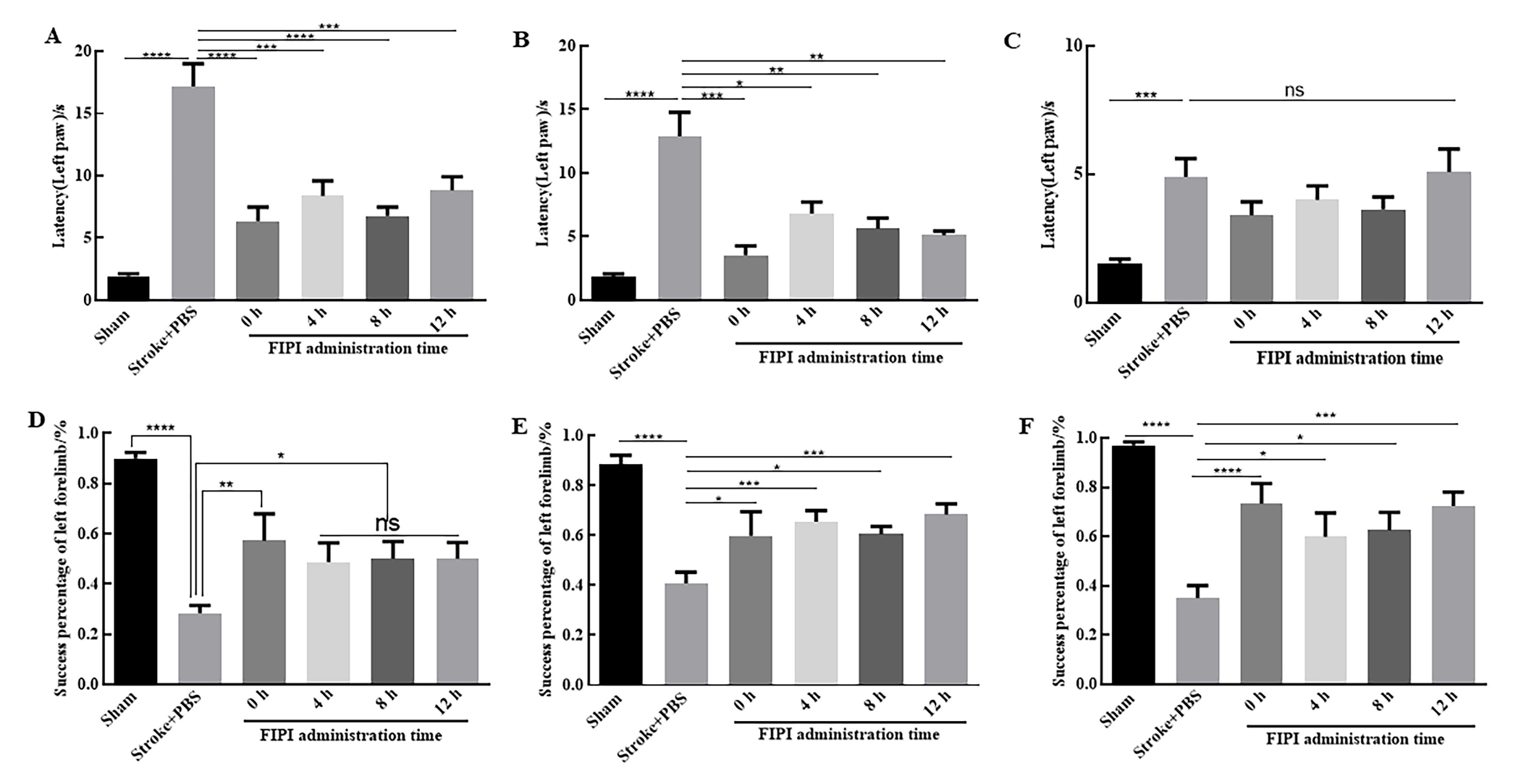
Figure 4 Behavior tests reveal the administration of 0.9 mg/kg FIPI at different time points after ischemic stroke can improve the neurological function of miceNote: A, B, and C denote adhesive removal tests (detecting latency time of left paw); D, E, and F are whisker tests (detecting success percentage of left forelimb). A and D show the behavior tests on the 1st day; B and E show the behavior tests on the 3rd day; C and F show the behavior tests on the 7th day. n=6 in each group. *P<0.05, **P<0.01, ***P<0.001, ****P<0.000 1; ns, not significant. FIPI, 5-fluoro-2-indolyl deschlorohalopemide, is a phospholipase D inhibitor.
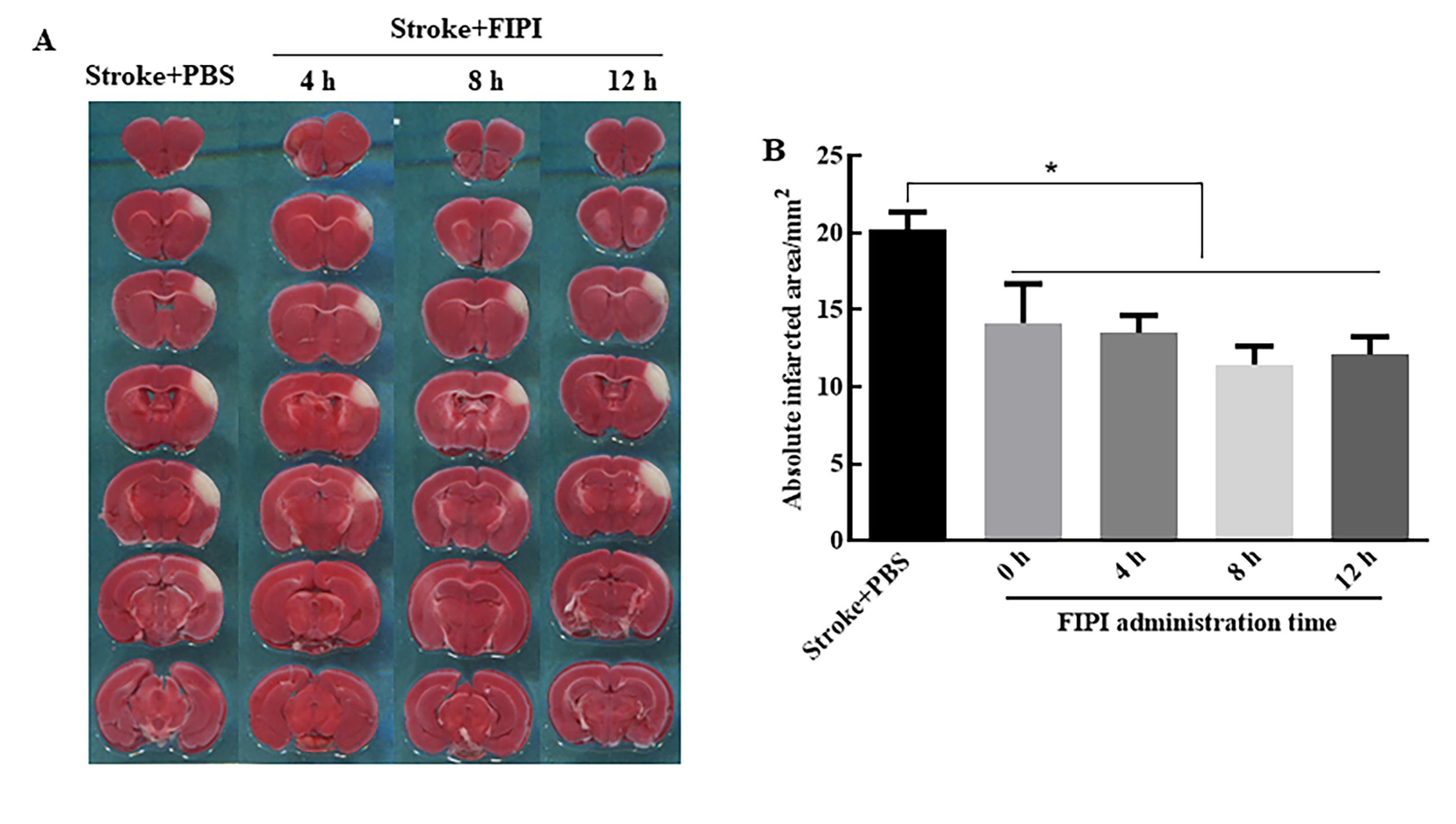
Figure 5 TTC staining reveals the administration of 0.9 mg/kg FIPI at different time points after ischemic stroke can reduce the volume of infarcted cortex of miceNote: A is the TTC staining of the infarcted cortex in different groups; white color indicates the infarcted cortex and red color indicates the normal cortex; B is the statistical analysis of the infarcted cortex volume (n=6 in each group,*P<0.05). FIPI, 5-fluoro-2-indolyl deschlorohalopemide, is a phospholipase D inhibitor.
| 1 | CAMPBELL B C V, DE SILVA D A, MACLEOD M R, et al. Ischaemic stroke[J]. Nat Rev Dis Primers, 2019, 5(1):70. DOI:10.1038/s41572-019-0118-8 . |
| 2 | WANG P, SHAO B Z, DENG Z Q, et al. Autophagy in ischemic stroke[J]. Prog Neurobiol, 2018, 163-164:98-117. DOI: 10.1016/j.pneurobio.2018.01.001 . |
| 3 | HWANG J Y, GERTNER M, PONTARELLI F, et al. Global ischemia induces lysosomal-mediated degradation of mTOR and activation of autophagy in hippocampal neurons destined to Die[J]. Cell Death Differ, 2017, 24(2):317-329. DOI:10.1038/cdd.2016.140 . |
| 4 | DALL'ARMI C, DEVEREAUX K A, DI PAOLO G. The role of lipids in the control of autophagy[J]. Curr Biol, 2013, 23(1): R33-R45. DOI:10.1016/j.cub.2012.10.041 . |
| 5 | PURI C, RENNA M, BENTO C F, et al. Diverse autophagosome membrane sources coalesce in recycling endosomes[J]. Cell, 2013, 154(6):1285-1299. DOI:10.1016/j.cell.2013.08.044 . |
| 6 | HUR J H, PARK S Y, DALL'ARMI C, et al. Phospholipase D1 deficiency in mice causes nonalcoholic fatty liver disease via an autophagy defect[J]. Sci Rep, 2016, 6:39170. DOI:10.1038/srep39170 . |
| 7 | DALL'ARMI C, HURTADO-LORENZO A, TIAN H, et al. The phospholipase D1 pathway modulates macroautophagy[J]. Nat Commun, 2010, 1:142. DOI:10.1038/ncomms1144 . |
| 8 | YOON M S. Vps34 and PLD1 take center stage in nutrient signaling: their dual roles in regulating autophagy[J]. Cell Commun Signal, 2015, 13:44. DOI:10.1186/s12964-015-0122-x . |
| 9 | ZHU Y B, KANG K, ZHANG Y, et al. PLD1 negatively regulates dendritic branching[J]. J Neurosci, 2012, 32(23):7960-7969. DOI:10.1523/jneurosci.5378-11.2012 . |
| 10 | ZHU Y B, GAO W, ZHANG Y, et al. Astrocyte-derived phosphatidic acid promotes dendritic branching[J]. Sci Rep, 2016, 6:21096. DOI:10.1038/srep21096 . |
| 11 | 陶少鑫, 朱彦兵, 于山平, 等. 小鼠缺血性脑卒中后磷脂酶D1在自噬和神经损伤中的作用[J]. 临床和实验医学杂志, 2019, 18(8): 790-794. DOI:10.3969/j.issn.1671-4695.2019.08.002 . |
| TAO S X, ZHU Y B, YU S P, et al. Role of phospholipase D1 in autophagy and neuronal damage after focal ischemic stroke in mice[J]. J Clin Exp Med, 2019, 18(8): 790-794. DOI:10.3969/j.issn.1671-4695.2019.08.002 . | |
| 12 | KLIER M, GOWERT N S, JÄCKEL S, et al. Phospholipase D1 is a regulator of platelet-mediated inflammation[J]. Cell Signal, 2017, 38:171-181. DOI:10.1016/j.cellsig.2017.07.007 . |
| 13 | SU W, YEKU O, OLEPU S, et al. 5-Fluoro-2-indolyl des-chlorohalopemide (FIPI), a phospholipase D pharmacological inhibitor that alters cell spreading and inhibits chemotaxis[J]. Mol Pharmacol, 2009, 75(3):437-446. DOI:10.1124/mol.108. 053298 . |
| 14 | HENKELS K M, MUPPANI N R, GOMEZ-CAMBRONERO J. PLD-specific small-molecule inhibitors decrease tumor-associated macrophages and neutrophils infiltration in breast tumors and lung and liver metastases[J]. PLoS One, 2016, 11(11): e0166553. DOI:10.1371/journal.pone.0166553 . |
| 15 | MAO L L, LI P Y, ZHU W, et al. Regulatory T cells ameliorate tissue plasminogen activator-induced brain haemorrhage after stroke[J]. Brain, 2017, 140(7):1914-1931. DOI:10.1093/brain/awx111 . |
| 16 | ANDREJEVA G, GOWAN S, LIN G, et al. De novo phosphatidylcholine synthesis is required for autopha-gosome membrane formation and maintenance during autophagy[J]. Autophagy, 2020, 16(6):1044-1060. DOI:10.1080/15548627.2019.1659608 . |
| 17 | CAI M, HE J, XIONG J, et al. Phospholipase D1-regulated autophagy supplies free fatty acids to counter nutrient stress in cancer cells[J]. Cell Death Dis, 2016, 7(11): e2448. DOI:10.1038/cddis.2016.355 . |
| 18 | TIAN F, DEGUCHI K, YAMASHITA T, et al. In vivo imaging of autophagy in a mouse stroke model[J]. Autophagy, 2010, 6(8):1107-1114. DOI:10.4161/auto.6.8.13427 . |
| 19 | MARCHESAN D, RUTBERG M, ANDERSSON L, et al. A phospholipase D-dependent process forms lipid droplets containing caveolin, adipocyte differentiation-related protein, and vimentin in a cell-free system[J]. J Biol Chem, 2003, 278(29):27293-27300. DOI:10.1074/jbc.m301430200 . |
| 20 | NGUYEN T B, OLZMANN J A. Lipid droplets and lipotoxicity during autophagy[J]. Autophagy, 2017, 13(11):2002-2003. DOI:10.1080/15548627.2017.1359451 . |
| 21 | MCDERMOTT M I, WANG Y, WAKELAM M J O, et al. Mammalian phospholipase D: function, and therapeutics[J]. Prog Lipid Res, 2020, 78:101018. DOI:10.1016/j.plipres. 2019.101018 . |
| 22 | BAE E J, LEE H J, JANG Y H, et al. Phospholipase D1 regulates autophagic flux and clearance of α-synuclein aggregates[J]. Cell Death Differ, 2014, 21(7):1132-1141. DOI:10.1038/cdd. 2014.30 . |
| 23 | OLIVEIRA T G, CHAN R B, TIAN H, et al. Phospholipase d2 ablation ameliorates Alzheimer's disease-linked synaptic dysfunction and cognitive deficits[J]. J Neurosci, 2010, 30(49):16419-16428. DOI:10.1523/jneurosci.3317-10.2010 . |
| 24 | KIM S H, PARK M Y, YUN N J, et al. Targeting PLD2 in adipocytes augments adaptive thermogenesis by improving mitochondrial quality and quantity in mice[J]. J Exp Med, 2022, 219(2): e20211523. DOI:10.1084/jem.20211523 . |
| 25 | YUZHU W, DAN T, CHANGWEI W, et al. Propofol attenuates α-synuclein aggregation and neuronal damage in a mouse model of ischemic stroke [J]. Neurosci Bull, 2020, 36(3):289-298. DOI:10.1007/s12264-019-00426-0 |
| [1] | Jia LIU, Yanrong YE, Yun SHEN, Qiying TANG, Meiqing CHEN, Kehui YI, Shaozhuang CHEN. Ginkgolide B Promotes Neural Function Recovery of Ischemic Stroke Mice by Regulating Characteristics of Brain T Cells and Their Interactions with Glial Cells [J]. Laboratory Animal and Comparative Medicine, 2024, 44(2): 139-148. |
| [2] | Bo DONG, Jiaxin LIU, Wei XIONG, Songqi TANG, Wei HUANG. Progress in Animal Models of Ischemic Stroke [J]. Laboratory Animal and Comparative Medicine, 2022, 42(1): 54-61. |
| [3] | SONG Binbin, DONG Wenzhou, JIA Bingquan, ZHEN Ran, PENG Yu, YANG Xuan, YU Jia. Expression and Distribution of Molecules Regulating Protein Degradation Pathway in Nervous System of Mice [J]. Laboratory Animal and Comparative Medicine, 2020, 40(6): 463-469. |
| [4] | HE Dawei, HE Aolin, ZHOU Minghui, YU Yaping, ZHANG Minghua. Effects of Sodium Oxalate on Autophagy and Apoptosis of Cholangiocarcinoma Cells#br# [J]. Laboratory Animal and Comparative Medicine, 2020, 40(5): 403-. |
| [5] | ZHU Huiqin, ZOU Yanqiong, YANG Jie, YI Jing, YANG Jie. Small Ubiquitin-like Modifier Specific Protease 3 Regulates Autophagy in Mouse Alveolar TypeⅡ Epithelial Cells [J]. Laboratory Animal and Comparative Medicine, 2020, 40(4): 270-. |
| [6] | MIAO Jia-ning, LIU Bo, DING Jing-jing, WANG Li-li. Effects of Fhl1 Knockout on the Differentiation and Autophagy in Gastrocnemius Muscle in Mice of Different Ages [J]. Laboratory Animal and Comparative Medicine, 2019, 39(4): 274-279. |
| [7] | LIANG Yong-jun, ZHANG Peng, WANG Yue-qian, GAO Li-li, CAO Ting, QIAO Zheng-dong. High-fat Diet Induced Type 2 Diabetes Mellitus and Obesity in C57BL/6 Mice [J]. Laboratory Animal and Comparative Medicine, 2016, 36(5): 361-364. |
| [8] | LI Yuan, ZHANG Mei-ying. Research Progress on Autophagy with Parkinson Disease and Related Models [J]. Laboratory Animal and Comparative Medicine, 2015, 35(4): 335-340. |
| [9] | ZHAO Shan-min, LIN Li-fang, XIAO Bang, WANG Yun-hui, GONG Chen, ZHANG Lu, YU Chen-lin, TANG Qiu, SUN Wei, CUI Shu-fang. Comparative Effects of Hypoxia on Autophagy and Apoptosis of Naked Mole Rat Fibroblasts [J]. Laboratory Animal and Comparative Medicine, 2014, 34(5): 405-410. |
| [10] | LIN Li-fang, XIAO Bang, ZHAO Shan-min, TANG Qiu, YU Chen-lin, SUN Wei, ZHANG Lu, CAI Li-ping, XU Chen, CHENG Ji-shuai, CUI Shu-fang. The Effect of Poly I:C on Autophagy of Naked Mole Rat [J]. Laboratory Animal and Comparative Medicine, 2014, 34(5): 411-416. |
| [11] | LIN Li-fang, ZHAO Yi-ning, ZHAO Shan-min, XU Chen, CUI Shu-fang. Comparative Study on Autophagy Regulation between Naked Mole Rat and C57BL/6 Mouse [J]. Laboratory Animal and Comparative Medicine, 2013, 33(4): 301-305. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||