
Laboratory Animal and Comparative Medicine
• XXXX XXXX •
GONG Leilei1( ), WANG Xiaoxia2, FENG Xuewei1, LI Xinlei1, ZHAO Han1, ZHANG Xueyan1(
), WANG Xiaoxia2, FENG Xuewei1, LI Xinlei1, ZHAO Han1, ZHANG Xueyan1( ), FENG Xin1(
), FENG Xin1( )
)
Online:2025-05-14
Contact:
ZHANG Xueyan, FENG Xin
CLC Number:
GONG Leilei,WANG Xiaoxia,FENG Xuewei,et al. Model and Mechanism of Action of Premature Ovarian Insufficiency Induced by Cyclophosphamide at Different Concentrations Based on SIRT5-FOXO3a Signaling Pathway[J]. Laboratory Animal and Comparative Medicine. DOI: 10.12300/j.issn.1674-5817.2024.194.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.slarc.org.cn/dwyx/EN/10.12300/j.issn.1674-5817.2024.194
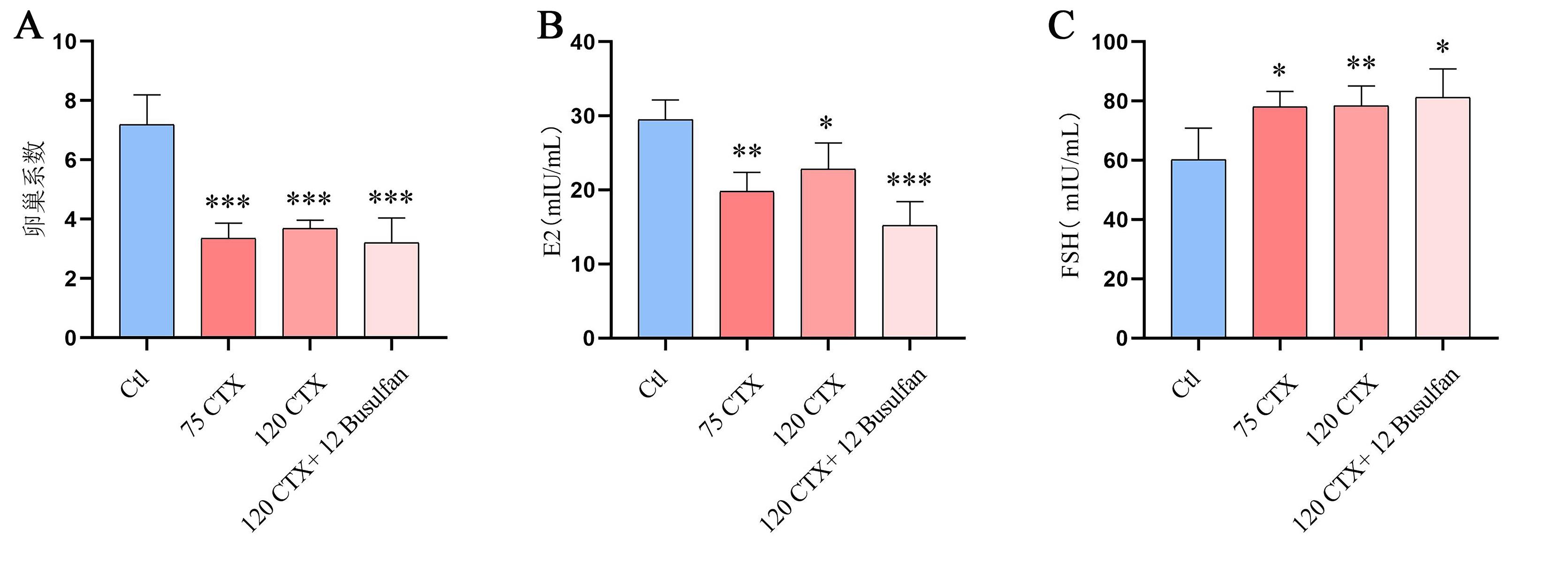
Figure 1 ovarian index and serum hormone change levels after CTX or CTX+Busulfan modelling.Note:Ctl represents control group; CTX represents Cyclophosphamide; Busulfan represents Busulfan; E2 represents Estradiol; FSH represents follicle-stimulating hormone; Compared with Ctl (n=8), *P<0.05; **P<0.01; ***P<0.001.
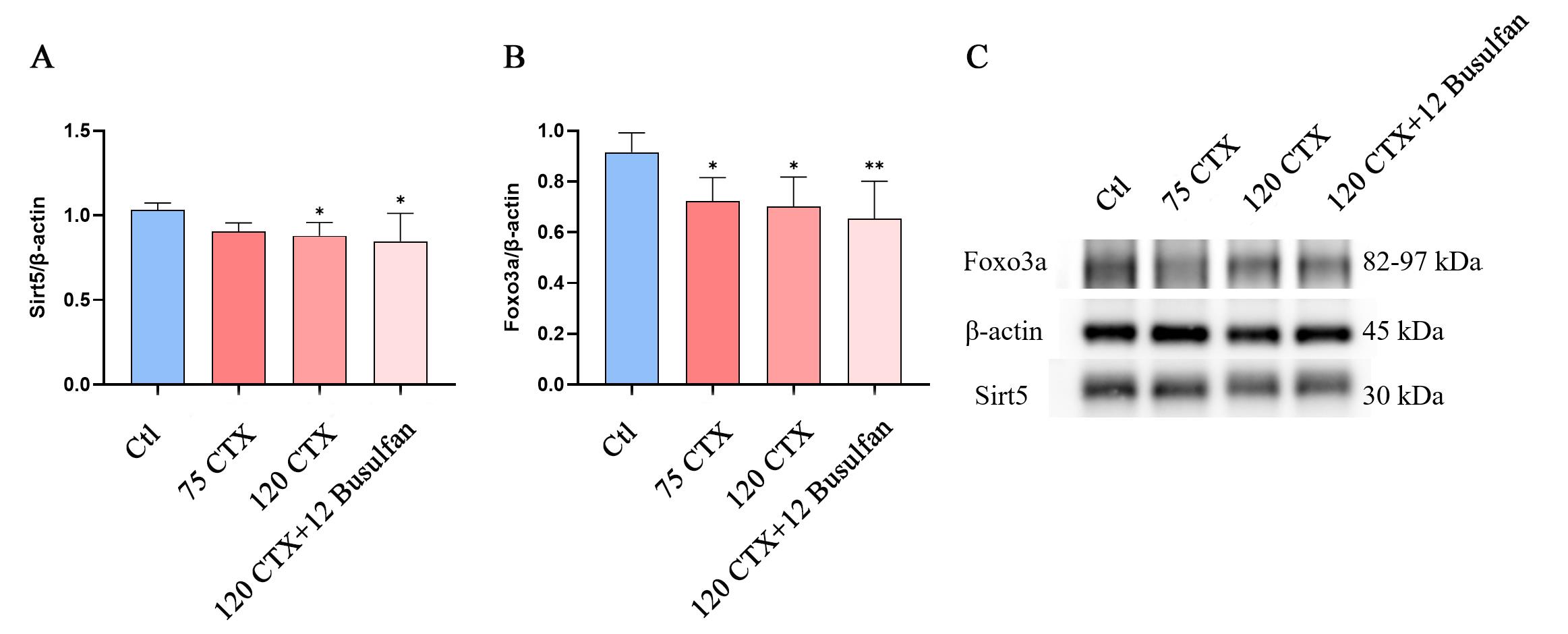
Figure 2 The expression of SIRT5 and FOXO3a in ovarian tissue after modelling with different concentrations of CTX and CTX+BusulfanNote:Ctl represents control group; CTX represents Cyclophosphamide; Busulfan represents Busulfan; Compared with Ctl (n=8), *P<0.05; **P<0.01.
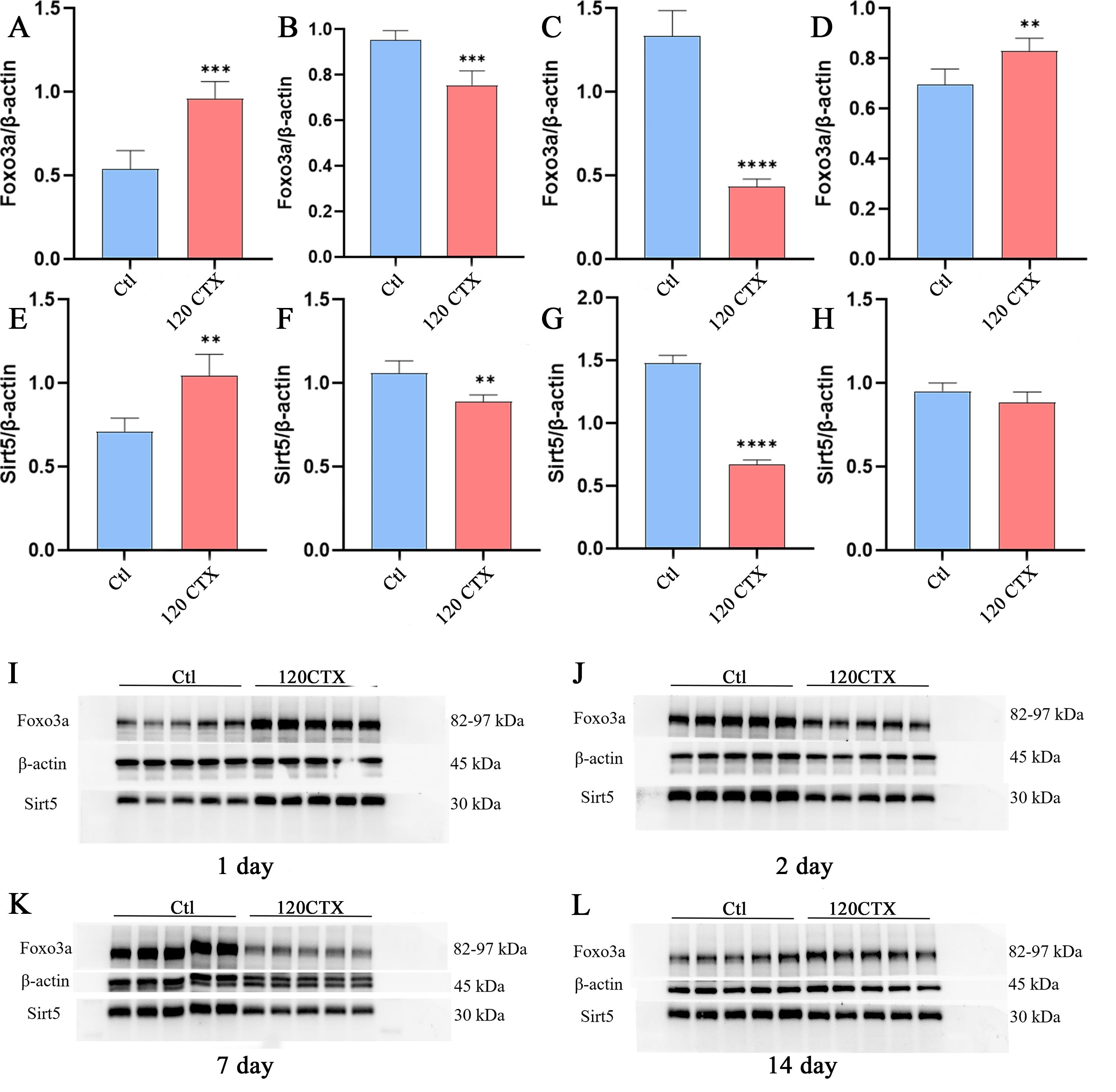
Figure 3 The expression of SIRT5 and FOXO3a in ovarian tissue at different times of 120 mg/kg CTX modellingNote:Ctl represents control group; 120 CTX represents 120 mg/kg CTX. A and E: The expression of FOXO3a and SIRT5 on day 1 post-modeling; B and F: The expression of FOXO3a and SIRT5 on day 2 post-modeling; C and G: The expression of FOXO3a and SIRT5 on day 7 post-modeling; D and I: The expression of FOXO3a and SIRT5 on day 14 post-modeling.
| 1 | 中华医学会妇产科学分会绝经学组. 早发性卵巢功能不全的临床诊疗专家共识(2023版)[J]. 中华妇产科杂志,2023,58(10):721-728. DOI: 10.3760/cma.j.cn112141-20230316-00122 . |
| 2 | PANAY N, ANDERSON R A, BENNIE A, et al. Evidence-based guideline: premature ovarian insufficiency [J]. Hum Reprod Open, 2024, 2024(4):hoae065. DOI: 10.1093/hropen/hoae065 . |
| 3 | 中华医学会妇产科学分会绝经学组. 早发性卵巢功能不全的临床诊疗专家共识(2023版)[J]. 中华妇产科杂志,2023,58(10):721-728. DOI: 10.3760/cma.j.cn112141-20230316-00122 . |
| 4 | 中国中西医结合学会妇产科专业委员会. 早发性卵巢功能不全中西医结合诊疗指南[J]. 中医杂志,2022,63(12):1193-1198. DOI:10. 13288/j. 11-2166/r. 2022. 12. 017 . |
| 5 | LI M, ZHU Y, WEI J, et al. The global prevalence of premature ovarian insufficiency: a systematic review and meta-analysis [J]. Climacteric,2023,26(2):95-102. DOI: 10.1080/13697137.2022.2153033 . |
| 6 | 吴洁,郁琦. 早发性卵巢功能不全的诊断和处理[J]. 中华医学信息导报,2016,31(21):21. DOI:10.3760/cma.j.issn.1000-8039.2016.21.021 . |
| 7 | RUTH K S, DAY F R, HUSSAIN J, et al. Genetic insights into biological mechanisms governing human ovarian ageing[J]. Nature, 2021, 596(7872):393-397. DOI: 10.1038/s41586-021-03779-7 . |
| 8 | 王艳辉,唐丽,雷磊. 基于数据挖掘的早发性卵巢功能不全动物模型分析[J]. 中国实验方剂学杂志,2023,29(9):225-233. DOI: 10.13422/j.cnki.syfjx.20230317 . |
| 9 | HUANG C Z, ZHAO S M, YANG YJ, et al. TP63 gain-of-function mutations cause premature ovarian insufficiency by inducing oocyte apoptosis [J]. J Clin Invest, 2023, 133(5):e162315. DOI: 10.1172/JCI162315 . |
| 10 | FANOURIAKIS A, KOSTOPOULOU M, CHEEMA K, et al. 2019 Update of the Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis[J]. Ann Rheum Dis, 2020,79(6):713-723. DOI: 10.1136/annrheumdis-2020-216924 . |
| 11 | QIN X S, ZHAO Y, ZHANG T Y, et al. TrkB agonist antibody ameliorates fertility deficits in aged and cyclophosphamide-induced premature ovarian failure model mice[J]. Nat Commun, 2022, 13:914. DOI: 10.1038/s41467-022-28611-2 . |
| 12 | DING C Y, ZHU L P, SHEN H, et al. Exosomal miRNA-17-5p derived from human umbilical cord mesenchymal stem cells improves ovarian function in premature ovarian insufficiency by regulating SIRT7[J]. Stem Cells, 2020, 38(9):1137-1148. DOI: 10.1002/stem.3204 . |
| 13 | LI M Y, ZHANG D, ZHOU X W, et al. Cell-free fat extract improves ovarian function and fertility in mice with premature ovarian insufficiency[J]. Stem Cell Res Ther, 2022, 13:320. DOI: 10.1186/s13287-022-03012-w . |
| 14 | MO J H, HOU H, LI P D, et al. Human hair follicle-derived mesenchymal stem cells improve ovarian function in cyclophosphamide-induced POF mice [J]. Stem Cell Res Ther, 2025, 16(1):67. DOI: 10.1186/s13287-024-04097-1 . |
| 15 | BHARDWAJ J K, BIKAL P, SACHDEVA S N. Chemotherapeutic drugs induced female reproductive toxicity and treatment strategies [J]. J Biochem Mol Toxicol, 2023, 37(7): e23371. DOI: 10.1002/jbt.23371 . |
| 16 | SWIGONSKA S, NYNCA A, MOLCAN T, et al. The Role of lncRNAs in the Protective Action of Tamoxifen on the Ovaries of Tumor-Bearing Rats Receiving Cyclophosphamide[J]. Int J Mol Sci, 2024, 25(23):12538. DOI: 10.3390/ijms252312538 . |
| 17 | YAO Y, WANG B, YU KH, et al. Nur77 ameliorates cyclophosphamide-induced ovarian insufficiency in mice by inhibiting oxidative damage and cell senescence[J]. J Ovarian Res, 2024, 17(1):203. DOI: 10.1186/s13048-024-01532-y . |
| 18 | LANDE Y, FISCH B, TSUR Aet al. Short-term exposure of human ovarian follicles to cyclophosphamide metabolites seems to promote follicular activation in vitro[J]. Reprod Biomed Online, 2017, 34:104–114. DOI: 10.1016/j.rbmo.2016.10.005 . |
| 19 | YUKSEL A, BILDIK G, SENBABAOGLU, et al. The magnitude of gonadotoxicity of chemotherapy drugs on ovarian follicles and granulosa cells varies depending upon the category of the drugs and the type of granulosa cells[J]. Hum Reprod, 2015, 30:2926–2935. DOI: 10.1093/humrep/dev256 . |
| 20 | DI EMIDIO G, D'AURORA M, PLACIDI M, et al. Pre-conceptional maternal exposure to cyclophosphamide results in modifications of DNA methylation in F1 and F2 mouse oocytes: evidence for transgenerational effects[J]. Epigenetics, 2019, 14(11):1057-1064. DOI: 10.1080/15592294.2019.1631111 . |
| 21 | PETRILLO S K, DESMEULES P, TRUONG T Q, et al. Detection of DNA damage in oocytes of small ovarian follicles following phosphoramide mustard exposures of cultured rodent ovaries in vitro[J]. Toxicol Appl Pharmacol, 2011, 253:94–102. DOI: 10.1016/j.taap.2011.03.012 . |
| 22 | AI G H, MENG M, GUO J, et al.Adipose-derived stem cells promote the repair of chemotherapy-induced premature ovarian failure by inhibiting granulosa cells apoptosis and senescence [J]. Stem Cell Res Ther, 2023, 14(1):75. DOI: 10.1186/s13287-023-03297-5 . |
| 23 | LUAN Y, EDMONDS M E, WOODRUFF T K, et al. Inhibitors of apoptosis protect the ovarian reserve from cyclophosphamide[J]. J Endocrinol, 2019, 240:243–256. DOI: 10.1530/JOE-18-0370 . |
| 24 | NGUYEN Q N, ZERAFA N, LIEW S H, et al. Loss of PUMA protects the ovarian reserve during DNA-damaging chemotherapy and preserves fertility[J]. Cell Death Dis, 2018,9:618. DOI: 10.1038/s41419-018-0633-7 . |
| 25 | JEELANI R, KHAN S N, SHAEIB F, et al. Cyclophosphamide and acrolein induced oxidative stress leading to deterioration of metaphase II mouse oocyte quality[J]. Free Radic Biol Med, 2017, 110: 11–18. DOI: 10.1016/j.freeradbiomed.2017.05.006 . |
| 26 | CHEN Y, ZHAO Y, MIAO C Y, et al. Quercetin alleviates cyclophosphamide-induced premature ovarian insufficiency in mice by reducing mitochondrial oxidative stress and pyroptosis in granulosa cells[J]. J Ovarian Res, 2022, 15:138. DOI: 10.1186/s13048-022-01080-3 . |
| 27 | GONG L L, HOU J L, YANG H J, et al. Kuntai capsule attenuates premature ovarian insufficiency by activating the FOXO3/SIRT5 signaling pathway in mice: A comprehensive study using UHPLC-LTQ-Orbitrap and integrated pharmacology[J]. J Ethnopharmacol, 2024, 322:117625. DOI: 10.1016/j.jep.2023.117625 . |
| 28 | CASTRILLON D H, MIAO L, KOLLIPARA R, et al. Suppression of ovarian follicle activation in mice by the transcription factor Foxo3a[J]. Science, 2003, 301(5630):215-218. DOI: 10.1126/science.1086336 . |
| 29 | PACELLA-LNCE L, ZANDER-FOX D L, LANE M. Mitochondrial SIRT5 is present in follicular cells and is altered by reduced ovarian reserve and advanced maternal age[J]. Reprod Fertil Dev, 2014, 26(8):1072-1083. DOI: 10.1071/RD13178 . |
| 30 | KUMAR S, LOMBARD D B. Functions of the sirtuin deacylase SIRT5 in normal physiology and pathobiology[J]. Crit Rev Biochem Mol Biol, 2018, 53(3): 311–334. DOI: 10.1080/10409238.2018.1458071 . |
| 31 | WANG Y F, ZHU Y B, XING S G, et al. SIRT5 prevents cigarette smoke extract-induced apoptosis in lung epithelial cells via deacetylation of FOXO3[J]. Cell Stress Chaperones, 2015, 20(5):805-810. DOI: 10.1007/s12192-015-0599-7 . |
| [1] | Fangqi BAO, Haiye TU, Mingsun FANG, Qian ZHANG, Minli CHEN. Advances in Research on Pathological and Molecular Mechanism of Hyperuricemic Nephropathy Based on Animal Models [J]. Laboratory Animal and Comparative Medicine, 2024, 44(2): 180-191. |
| [2] | Tingting FENG, Yitong LI, Yue WU, Jue WANG, Qi KONG. Transcriptome Data and Comparative Medical Analysis of COVID-19 Virus Infection [J]. Laboratory Animal and Comparative Medicine, 2024, 44(1): 62-73. |
| [3] | Taofeng LU, Hui ZHANG, Jie ZHOU, Qian LI, Shuguang WU, Yanjun WU. Effects of Pogostemon cablin on Serum Metabolomiceof Guizhou Miniature Pigs and It's mechanism [J]. Laboratory Animal and Comparative Medicine, 2023, 43(3): 253-261. |
| [4] | Jingwei MA, Gen LI, Yang YANG, Caixia ZANG, Xiuqi BAO, Dan ZHANG. Comparative Study on Different Recovery Periods of the Spermatogenic Dysfunction Mouse Model Induced by Cyclophosphamide [J]. Laboratory Animal and Comparative Medicine, 2023, 43(2): 112-123. |
| [5] | LUO Jianbo, LI Junhui, WANG Haijiang, ZHOU Xiaoyu, ZENG Tao, ZHOU Jia, ZHU Xianjun. Metabolic Disease Animal Models induced by High-fat Diets [J]. Laboratory Animal and Comparative Medicine, 2021, 41(1): 70-78. |
| [6] | LIU Xiaoyu, LU Xuancheng, CHEN Hongyan, LU Shengming, LI Genping, HE Zhengming. Practice and Enlightenment of Management Mechanism of Laboratory Animals under Different Systems at Home and Abroad [J]. Laboratory Animal and Comparative Medicine, 2020, 40(4): 263-. |
| [7] | DONG Guoju, LIU Jiangang, Guan Jie. The Research Progress of Pathological Characteristics of Animal Models with Heart Failure with Ejection Fraction Preservation [J]. Laboratory Animal and Comparative Medicine, 2020, 40(1): 74-79. |
| [8] | ZHOU Jie, ZHAO Li-juan, TAO Ling-yun, HU Jian-hua, GAO Cheng. Research Progress on Infection Mechanism and Diagnostic Methods of Ectromelia Virus [J]. Laboratory Animal and Comparative Medicine, 2018, 38(2): 160-164. |
| [9] | SONG Ying, GUO Ya-juan, HUANG Ming-qian, LIANG Jin-qiang, HUANG Zhi-ying. Effect of Different Factors on Cyclophosphamide Induced Immunosuppression Mice Model [J]. Laboratory Animal and Comparative Medicine, 2017, 37(1): 36-39. |
| [10] | XU Long-jin, WANG Kou-zhou. Screening of Mouse Strain Susceptive to Chronic Stress Depression and Preliminary Research on Its Mechanism [J]. Laboratory Animal and Comparative Medicine, 2016, 36(4): 257-262. |
| [11] | GU Yun-hao, CAO Chen-jie, HU Bi-yuan, WANG Jun, HAN Dong-dong, XU Ai-hua. Establishment of S180 Tumor Multidrug Resistance Mouse Model by Increasing PFC and Observation on Stability [J]. Laboratory Animal and Comparative Medicine, 2015, 35(5): 367-373. |
| [12] | GAO Jie, HE Zheng-ming. Research Progress of Murine Norovirus in Characteristics, Immunology and Detection Methods [J]. Laboratory Animal and Comparative Medicine, 2015, 35(5): 414-420. |
| [13] | WANG Xiao-jie, ZHANG Zhi-jun, YE Dong-qing. Genetic Engineering Mice Models of Depressive-like or Depression-resistant Phenotype [J]. Laboratory Animal and Comparative Medicine, 2015, 35(2): 142-148. |
| [14] | LI Hao, JI Guo-xia, WANG Ke-zhou, JI Chuan-liang, LI Lan-bo, ZHANG Yan, FENG Mo-zhu, LI Jian-mei, LIU Tao. The Influence of Colla Corii Asini on Growth and Quality of Hair in Mice Treated by Cyclophosphamide [J]. Laboratory Animal and Comparative Medicine, 2015, 35(1): 17-22. |
| [15] | SHAO Guo-yan, XIE Jian-yun, GAO Cheng. Progress on Immune Mechanism of Microtus fortis in Protecting against Schistosoma japonicum Infection [J]. Laboratory Animal and Comparative Medicine, 2013, 33(3): 243-246. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||